Falls are multi-factorial in nature which makes them tricky to manage but thanks to a new systematic review we know the top 5 things to include in your assessment and treatment plans.
Falls assessment and prevention always presents a challenge in clinical practice. The multi-factorial nature of the numerous causes for falls means it can become overwhelming when trying to decide which risk needs the most attention when you’re assessing and treating someone who either falls or might fall in the future.
Learn Which Exercises Prevent Falls
This complexity means numerous clinical guidelines exist all aiming to tell you what you should focus on during your assessment and which treatments you should use. Thankfully a new systematic review published in JAMA has evaluated the best guidelines and synthesised the recommendations from the best guidelines into one easy to use list of recommendations for you to use in clinical practice.
Methods
This systematic review adhered to PRISMA guidance and the protocol was published in PROSPERO both signs of a good methodological rigour.
The search terms used for the eight databases used for the search included falls, clinical practice guidelines, management and prevention and older adults. The full strategy is available in full.
To be included within the review studies had to:
- evaluate the outcome of guidelines related to fall reduction, prevention and management
- involve clinical practice guidelines for preventing or managing falls
- focus on an elderly population
There were no restrictions on date, language or setting.
Articles were screened and assessed for inclusion by three independent reviewers with disagreement resolved through consensus. Quality of included guidelines was evaluated by using the AGREE-II tool which is bespoke to the evaluation of guidelines. Confidence in findings was assessed using GRADE.
Results
In total, from an initial search yield of 11,414 records, 15 were included within the final synthesis and results.
The AGREE-II scores across all of the 15 included studies shows high scores across all domains of the tool. There were two domains which were not scored as high, there were the involvement of patients as stakeholders and representation of professionals from diverse backgrounds and applicability of recommendations.
Recommendations and Agreement Across Guidelines
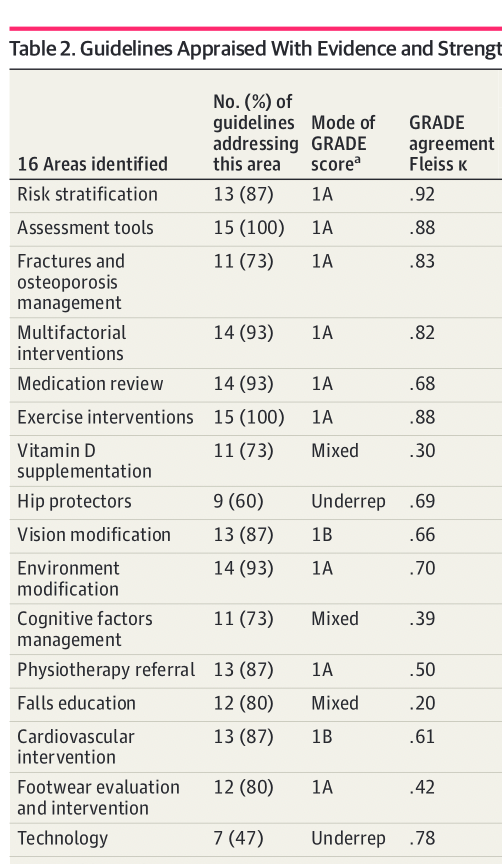
From the 15 guidelines included within the review there were 198 recommendations for falls prevention and management which were grouped into 16 topic areas and ranked based on their agreement, GRADE scores and consistency in recommendation. The list of these 16 topic areas with their GRADE score and agreement is shown below.
According to these results the two must important things to include within your clinical practice are assessing those who have a risk of falls and using exercise interventions to prevent falls. Other recommendations with high levels of agreement include medication review, multi-factorial interventions, osteoporosis assessment and environmental modification.
Inconsistent / Underrepresented Topic Areas in Recommendations
Vitamin D supplementation had a low level of agreements across the 15 guidelines included within the review. Seven guidelines strongly recommended the use of vitamin d supplementation, four weakly recommended the use and four guidelines didn’t mention supplementation.
There was a similar level of disagreement about the use of education on falls prevention for patients and caregivers which is a surprise considering the logical nature of doing so. However it’s possible that this disagreement reflects the complex nature of falls and that to have effective interventions multi-professional advice is required rather than simple solutions.
Unsurprisingly the use of hip protectors had low levels of agreement and for some reason remains a recommendation in some guidelines despite there being almost no empirical evidence to support the use. The recommendation in some guidelines is likely as a last resort / if nothing else is working then try these kind of solution.
What is surprising is that the use of technology also has low levels of agreement however this is likely a reflection of the wide variety of what studies define as technology.
Risk Stratification
Most of the guidelines included within the review recommend the use of risk stratification using self-reported questions such as falls history, fear of falling and reserving gait and balance testing for those who screen positive on these questions.
Risk stratification algorithms are often used however there is a lack of agreement between the most commonly used algorithms.
For those who screen positive on the self-reported falls history several guidelines stratify risk by demographic factors or clinical characteristics such as balance and gait. The assessment of balance and gait using TUG, Berg Balance Scale and Tinetti was strongly recommended.
Conclusions and Summary
In your clinical practice the top 5 things to include within your assessment and management for those who are at risk of falls are: risk stratification, specific assessment for those who are at risk of falling, use of exercise for intervention, assessment for osteoporosis and adopting a multifactorial approach.