An editorial in this months edition of the BJSM has gathered considerable positive attention on social media this week for smashing apart the common misconceptions that are associated with back pain. Unhelpful beliefs surrounding back pain are rife within our industry and within the media which reinforces bad habits and incorrect management strategies. The unhelpful beliefs have been strongly proven to lead to greater levels of pain, disability, lower levels of productivity, opiate use and over medicalisation.
There probably isn’t another musculoskeletal conditon which has quite as many myths as back pain, but thanks to the work of these authors we, as a profession, are slowly correcting the narrative.
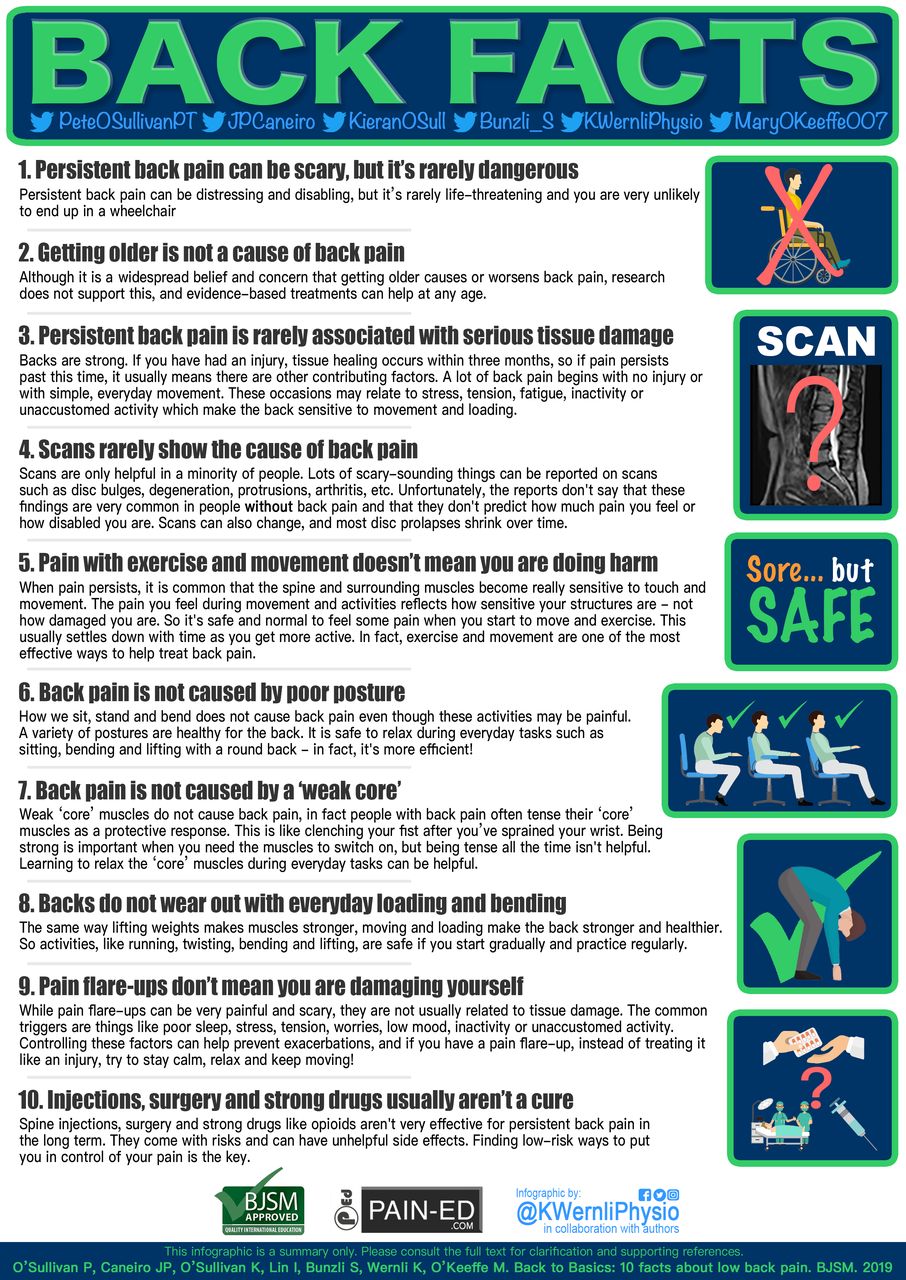
FACTS
- LBP is not a serious life-threatening medical condition.
- Most episodes of LBP improve and LBP does not get worse as we age.
- A negative mindset, fear-avoidance behaviour, negative recovery expectations, and poor pain coping behaviours are more strongly associated with persistent pain than is tissue damage.
- Scans do not determine prognosis of the current episode of LBP, the likelihood of future LBP disability, and do not improve LBP clinical outcomes.
- Graduated exercise and movement in all directions is safe and healthy for the spine.
- Spine posture during sitting, standing and lifting does not predict LBP or its persistence.
- A weak core does not cause LBP, and some people with LBP tend to overtense their ‘core’ muscles. While it is good to keep the trunk muscles strong, it is also helpful to relax them when they aren’t needed.
- Spine movement and loading is safe and builds structural resilience when it is graded.
- Pain flare-ups are more related to changes in activity, stress and mood rather than structural damage.
- Effective care for LBP is relatively cheap and safe. This includes: education that is patient-centred and fosters a positive mindset, and coaching people to optimise their physical and mental health (such as engaging in physical activity and exercise, social activities, healthy sleep habits and body weight, and remaining in employment).
One of the authors of the editorial is Peter O’Sullivan whose work around improving commuication with those suffering from low back pain we have featured on Physiospot before. It is well worth checking out and the infographic compliments the resource perfectly. Peter also has an excellent video too.
10 Helpful Back Facts Infographic
The infogrpahic included within the article is great as it focusses on the FACTS not the MYTHS. It is always easy to focus on the myths and why they are wrong but unfortuantely this often makesTreatments such as strong medications, injections and surgery are effective, and necessary, to treat LBP.the myth the centre of attention giving it more attention instead of dispelling it.
If you are interested in learning more about why these myths exist and what the correct way of managing back pain is make sure you check out the links to Physiopedia and Physioplus resources below.
