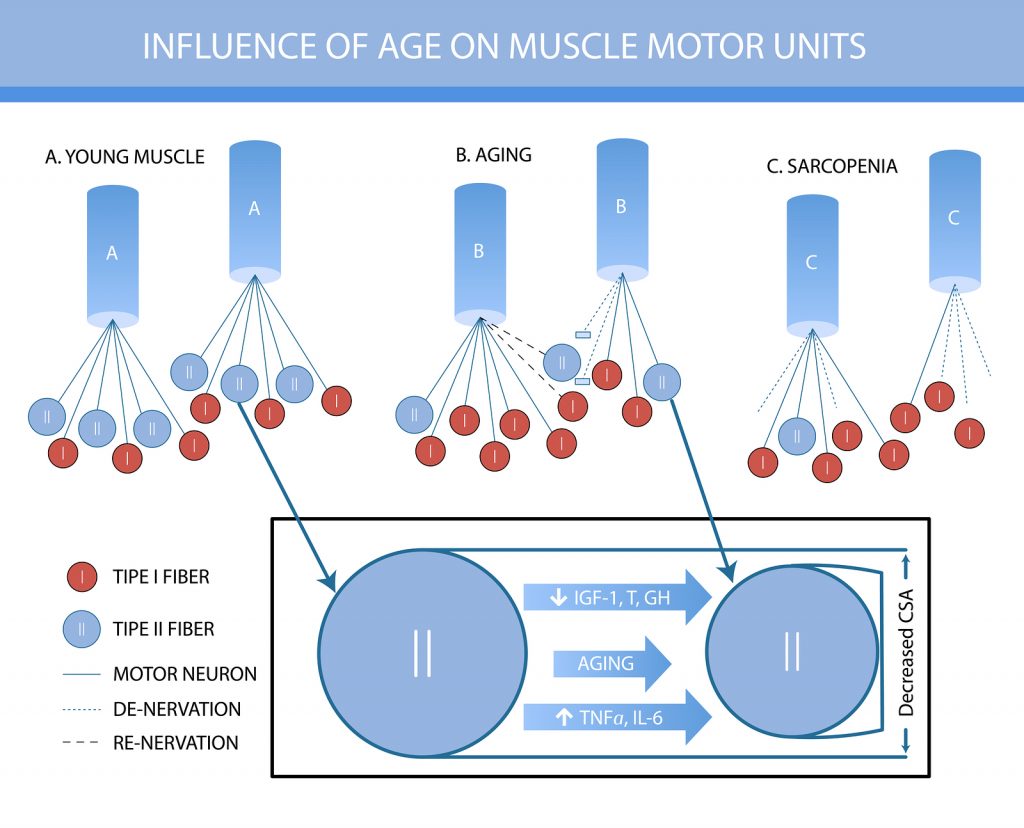
Sarcopenia should be thought of as a disease; acute or chronic muscle failure. The disease process is complex and not fully understood but we have come a long way in the decade between EWGSOP 1 and now. This is why the group have met again and updated their European Consensus on Definition and Diagnosis of Sarcopenia.
One of the drivers for meeting again was that a lot of research has been published in the past decade which has drastically improved our understanding of the condition. Unfortunately a lot of the research hasn’t translated to clinical practice this was the key task of the group, to provide clarity of definition and diagnosis.
Definition
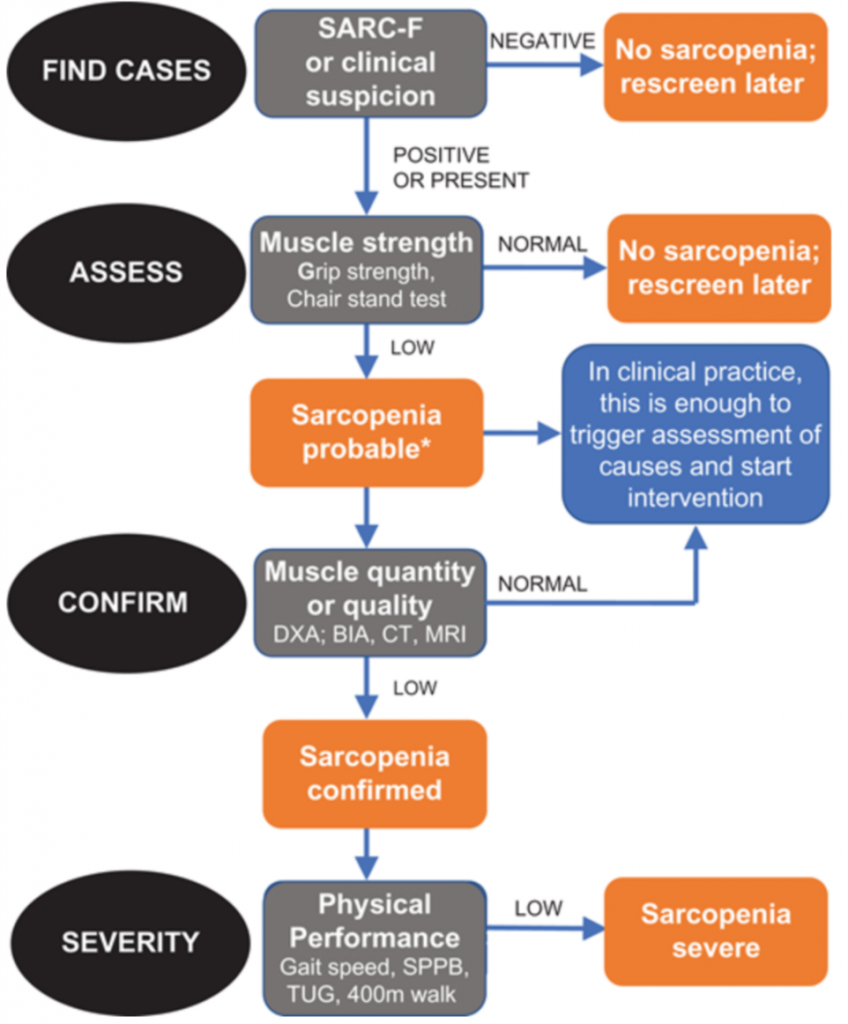
Probable sarcopenia is identified if the individual has low muscle strength as well as having either low muscle quantity/quality or low physcial performance.
The difference between this new operational diagnosis and the definition used in EWGSOP 1 is that there is now a focus on the presence of low muscle strength as the defining characteristic. This is not to say this alone is the only sign required to diagnose the condition. The muscle architecture needs to be considered as well as the performance of the fibres themselves. We can all think of a frail older person who is super strong.
If low strength, low quality and low performance are all present then the sarcopenia is considered severe.
Recommended Validated Tools for Diagnosis
The SARC-F Questionnaire is what EWGSOP 2 recommends for characterisation of sarcopenia. This is a 5-item self-reported questionnaire that has low-moderate sensitivity and very high specificity. It is inexpensive and convenient and will ensure that clinicians identify severe cases of sarcopenia. Therefore it is a great tool to start to introduce the concept of muscle failure into clinical practice.
There are a number of other investigations that can reliably quantify the severity of muscle loss but they are expensive and unavailable to 99% of practicing clinicians. They are interesting nonetheless and are likely to become more commonplace in the future.
Take Lumbar 3rd Vertebrae CT scans as an example. L3-CT correlates significantly with whole body muscle mass as well as accurately predicting prognosis. CT is also useful for investigating mid-thigh muscle mass which is potentially more accurate than L3-CT.
A cheaper and just as accurate alternative to CT is diagnostic ultrasound and is highly reliable. US will also inform the user of muscle thinckness, cross-sectional area, fascicle length, pennation angle and echogenicity, all of which surely makes all physios jump at joy. The European Geriatric Medical Society produces a consensus protocol for the use of US in sarcopenia so in all liklihood this will be used in the near future, at least in research, the diagnose sarcopenia.
Measurement of Sarcopenia
IThis is relatively simple to do through the use of a hand grip dynamometer and the SPPB. Grip strength is a great indicator of poor patient outcomes and prolonged hospital stays and the SPPB (Short Physcial Performance Battery) means whole body function is considered in each individual.
Other Key Points
Two other considerations when assessing sarcopenia is the consideration of whether it is primary or secondary. Sarcopenia is considered primary if no other causes are indentified other it being a result of age. The changes seen in sarcopenia can be as a result of systemic disease, physical inactivity, disability, reduced calorific or protein intake or even anorexia and malabsorption syndromes, in all cases these would evoke secondary sarcopenia.
Also give thought to whether the person is exhibiting acute (<6 months) or chronic (>6 months). This is important as underlying chronic sarcopenia means that a person has an increased risk of mortality. This consideration of acuity also means that clinicans are more likely to monitor progression of the condition and help prevent and delay progression and poor outcome.
Conclusion
Sarcopenia is muscle failure; it can be acute or chronic and primary or secondary. It is caused by a number of different factors some of which are better understood than others. Either way our knowledge is improving rapidly and, with the addition of diagnostic tools which are readily available and inexpensive, the time has come for use to look the disease head on and do something about it. As physiotherapists sarcopenia is centre lane, it’s muscle failure and surely there isn’t a disease more appropriate for us to tackle.