We recently finished another round of our increasingly popular Volunteer Orientation Course. As part of the final assignment members were tasked to write an original piece of work to share with the profession, the contributions were of the highest quality. Below is the great piece of work written by Luciana Segantin Lopes.
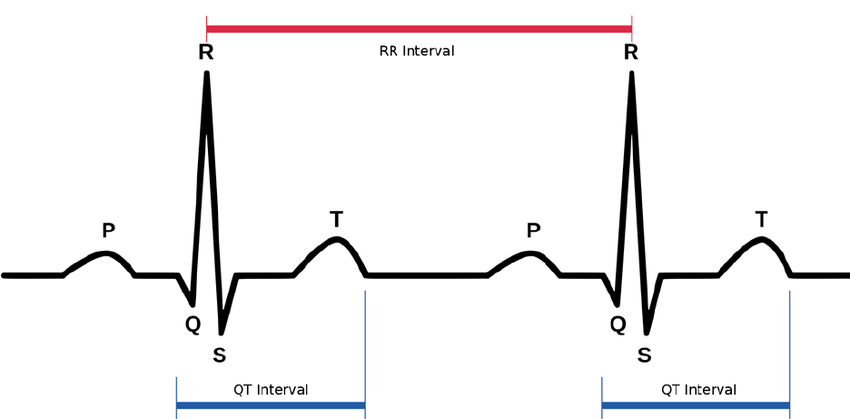
Heart Rate Variability (HRV) – is recognised as a versatile, promising, non-invasive marker of modulations of the autonomous nervous system (ANS) and reflects the changes in the interval between heartbeats (R wave) over time.
The autonomic nervous system regulates very important systems in our body, including heart and respiration rate and digestion. The autonomic nervous system has a parasympathetic (rest) and a sympathetic (activation) branch. Heart rate variability is an indicator that both branches are functioning – the parasympathetic in particular.
Intrinsic heart rate is measured in the condition in which neither parasympathetic nor sympathetic regulation is present. When completely blocked from autonomic regulation, a healthy heart contracts at a rate of about 100 beats per minute (the number is individual, though).
Parasympathetic regulation lowers your heart rate from the intrinsic level, giving more room for variability between successive heartbeats. Parasympathetic regulation causes almost immediate changes that affect only a few beats at a time, after which heart rate returns towards the intrinsic rate.
Sympathetic regulation elevates your heart rate from the intrinsic level, and there is less room for variability between successive heartbeats. Sympathetic regulation affects several consecutive heart beats.
The time between one R wave and the next, in milliseconds, is known as the R-R interval or the interval between beats.
This measurement is becoming more and more common in assessments of the presence of diseasesthe stratification of risk, autonomic dysfunction and intervention results.
HRV analysis provides a perspective of the function of the sympathetic and parasympathetic nervous systems as it is mainly controlled by the continuous interaction of the ANS.
Two components of frequency are usually distinguishable in the short-term HRV: high frequency (HF) and low frequency (LF). In normal resting conditions and healthy individuals, the parasympathetic route is dominant, resulting in a high HRV, whereas a lower HRV and health problems have been associated with an increase in sympathetic activity while at rest.
Put these together and we can formulate a rule that when the rest-related parasympathetic branch is active and the sympathetic branch is inactive, your heart rate is lower and HRV higher. Factors such as stress can lead to the withdrawal of parasympathetic activity, or activation of sympathetic branch even when you are resting, both leading to elevated heart rate and lowered HRV.
HRV and Aspects of Mental Health
There is interest in HRV in the field of psychophysiology. For example, HRV is related to emotional arousal. High-frequency (HF) activity has been found to decrease under conditions of acute time pressure and emotional strain and elevated state anxiety, presumably related to focused attention and motor inhibition.
HRV has been shown to be reduced in individuals reporting to worry more. In individuals with post-traumatic stress disorder (PTSD), HRV and its HF component (see below) are reduced whilst the low-frequency (LF) component is elevated. Furthermore, PTSD patients demonstrated no LF or HF reactivity to recalling a traumatic event.
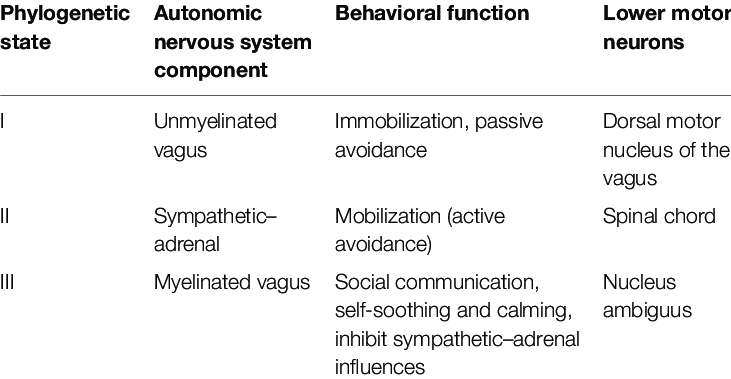
The Polyvagal Theory
The Polyvagal Theory describes pathways in the autonomic nervous system that mediate HRV. This theory emphasises the role of heart rate variability in understanding the magnitude and nature of vagal outflow to the heart. This theory decomposes heart rate variability based on frequency domain characteristics with an emphasis on respiratory sinus arrhythmia and its transmission by a neural pathway that is distinct from other components of HRV. There is anatomic and physiological evidence for a polyvagal control of the heart.
HRV and Cardiovascular Training.
When you start regular cardiovascular training, one of the fastest positive adaptations of your body is increased blood plasma volume, and subsequently increased stroke volume. As a result, your heart can keep the blood flowing and maintain adequate blood pressure at a lower heart rate. And as we remember, lower heart rate is regulated by the parasympathetic branch. Parasympathetic regulation causes longer interbeat intervals and elevated HRV. In the long term, regular exercise also strengthens the heart muscle, which once again means lower HR and higher HRV.
On the whole, high heart rate variability is an indication of especially cardiovascular, but also overall health as well as general fitness. Generally speaking, it tells us how recovered and ready we are for the day. Also, HRV can react to changes in our body even earlier than heart rate. This makes it a particularly sensitive tool that gives us insights into our wellbeing.
You might notice that a very intensive endurance exercise can acutely lower your HRV, but if you recover well, it will jump back up again soon. This is generally speaking a sign that your body handles the training load well. If your HRV doesn’t jump back up, you may have been training too hard or too often. Overall, it seems that regular endurance exercise does tend to increase HRV in the long run, and a high HRV value (compared to your baseline) means that your body should be ready for the next exercise.
General Rules to Remember When Working with HRV
- If you become stressed or don’t sleep well for a while, you could see your HRV values gradually dropping, indicating that your body might not be at its best, and you need to take some time for recovery.
- One interesting finding is that your HRV can jump down if you’re about to get sick – even before you develop any symptoms. If this is the case, and you can take it easy for a day or two, your body might fight off the disease. If you get sick, your HRV can stay quite low even after the symptoms are gone. This indicates that your body is still recovering, and isn’t ready for maximal performances.
- Smoking and alcohol consumption can reduce HRV. So, you will most probably notice that your HRV goes down momentarily after a night out in town.
- If you’re an endurance athlete or otherwise exercise-oriented, these research findings* might interest you: among recreational endurance athletes, it seems that the level of HRV predicts training response for several weeks of training. If you have high HRV, your body can be expected to respond positively to high-intensity training. If you have low HRV, your body can be expected to respond positively to a high volume of low-intensity training.
- Overall, HRV drops with dehydration, but jumps back to its baseline level with good hydration. As discussed, both exercise and alcohol can cause dehydration – as can long bouts in the sauna.
References
- Pereira, A., Et al. Assessment of Heart Rate Variability in Fibromyalgia after Micro-physiotherapy. MTP&RehabJournal 2014, 12:730-743.
- Hautala AJ, Kiviniemi AM, Makikallio TH, Kinnunen H, Nissilä S, Huikuri HV, Tulppo MP. Individual differences in the responses to endurance and resistance training. _Eur J Appl Physiol_ 2006;96(5):535–42.
- Vesterinen V, Häkkinen K, Hynynen E, Mikkola J, Hokka L, Nummela A. Heart rate variability in prediction of individual adaptation to endurance training in recreational endurance runners. Scand J Med Sci Sports 2013;23(2):171–80.
- Vesterinen V, Häkkinen K, Laine T, Hynynen E, Mikkola J, Nummela A. Predictors of individual adaptation to high-volume or high-intensity endurance training in recreational endurance runners. Scand J Med Sci Sports 2016;26(8):885–93.
By Luciana Segantin Lopes.
Over the coming weeks we’ll continue to share these writings with you. Let us know what you think!