As physiotherapists we are experts in rehabilitation. It is what we love doing but with healthcare budgets stretched, and waiting lists growing, it is difficult to see patient rehab from beginning to end. Let alone to see them thriving doing the things they once loved. What are the options for therapists working in the community or in acute hospitals to enable patients to thrive at home? Social prescribing may be part of the solution.
According to the King’s Fund social prescribing is:
“…a means of enabling GPs, nurses and other primary care professionals to refer people to a range of local, non-clinical services.”
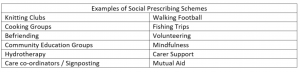
It is designed to help people with a range of social, mental-health, physical or functional needs that are otherwise unable to receive formal rehabilitation. This may be because they do not meet a criteria or because of inconsistent service provision. They are crucial to areas of healthcare with chronically underfunded primary care support such as mental health. John’s story (The Guardian) is an example of how the diversity of social prescribing greatly affected his life.
Another fine example of a voluntary service is AGE UK, who provide a wide range of services for older people in the UK. Without their volunteers a large number of vulnerable people would be lonely, unable to do their shopping and be susceptible crime. At the core of AGE UK are the principles the WCPT were trying to encourage on World PT Day this year; “Adding Life to Years”.
As with the area of mental health, there is a clear similarity between what physiotherapy in older people and social prescribing enterprises are trying to achieve. With many care visits being 15 minutes long there is not enough time to enable a person to achieve their higher activities of daily living. They are taken away from them or they are not achieved at all which contributes to delirium, undernourishment or immobility. This can reach a crisis point which causes a person to seek emergency help often in the form of a visit it ED. As shown by a study conducted in Rotherham (UK) social prescribing can reduce the rate of this occurring.
Many new and innovative services never make it past the pilot stage of their funding as they are deemed to be unsuccessful in terms of saving money for hospitals or councils. It is hard to argue against the benefits of a walking group for persons with diabetes or a post total knee replacement. In many of these cases it could be argued that the wrong key performance indicator is measured. Can these services really be assessed in the same was as hospital or healthcare led services?
Perhaps with the guidance of physiotherapists these services could have the clinical evidence base behind them to enable a more permanent status. After all couldn’t they be seen as similar services to that led by physiotherapy assistants or classes within hospital?
Do you use social prescribing in your daily practice or do you think it is diluting what other healthcare professions are trying to achieve? Let us know in the comments below, via social media or email.