Breathing has drawn a lot of attention in the past decade. For something that’s mostly unconscious, it has become quite trendy. Different approaches discuss the magic of breathing, athletes are now taught how to coordinate the core with their breath, and the diaphragm has become one of the most talked about muscles since the Transverse Abdominus became in vogue back in the 90’s.
So what’s the big deal? Why is everyone jumping on the breathing wagon?
The reason why breathing has become so popular is because it’s a simple task that can improve many aspects of the human body – minimal inputs for maximal outputs. And it’s not just mechanical, breathing has widespread effects throughout the entire body; from improving someone’s deadlift personal record to helping alleviating someone’s anxiety and pain. Going over all the benefits of breathing is beyond the scope of this article, but understanding the 3 main systems of the body that breathing affects is a good place to start.
But before we go into the 3 systems, it’s important to quickly review efficient versus inefficient breathing. proper breathing versus poor breathing technique.
Efficient Breathing Pattern
- Abdominal distension
- 3-D lower rib cage expansion
- Apical filling
- Rhythmic, Even, Tidal Breathing
Inefficient Breathing Pattern
- Vertical Rib Displacement
- Paradoxical Abdominal Movement
- Hinge at T-L junction during inhale
- Excessive accessory muscle activity
- Hyperventilation
- Decreased Exhalation
3 Systems That Breathing Affects
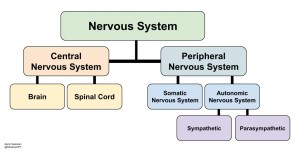 1) The Autonomous Nervous System
1) The Autonomous Nervous System
The autonomic nervous system (ANS) is involved in the physiological expression of stress. It responds to stressful stimuli (internal inputs, environment, physical movement, etc.) with either a sympathetic or parasympathetic response. Parasympathetic helps with the internal needs of homeostasis via the “rest & digest”response. Sympathetic mediates the interaction with the external environment with it’s “fight or flight”response. The resting state of the ANS can either be beneficial for overall health (parasympathetic) or detrimental (excessive/malapropos sympathetic). This depends on many variables, one of which is respiration.
The relationship between breathing and the ANS is described in Porges’book
- Expiration = Increased Vagal Activity = Increased Parasympathetic = Decreased Heart Rate
- Inspiration = Decreased Vagal Activity = Increased Sympathetic = Increased Heart Rate
Through this Brainstem-Respiratory Mechanism, breathing can have a major influence on your autonomic nervous system.
Inefficient Breathing (Hyperventilation)
With poor breathing patterns, you will often have increased inspiration (sympathetic) and decreased expiration (parasympathetic). This drives the ANS into a sympathetic state.
Efficient Breathing
With proper breathing patterns, your exhale (parasympathetic) is longer than your inspiration (sympathetic). This helps drive the ANS into a parasympathetic state.
So you can drive the ANS to either side of the continuum, just by breathing.
 2) Circulation: Improves Blood Flow and Oxygenation to Tissues
2) Circulation: Improves Blood Flow and Oxygenation to Tissues
When it comes to healing injuries, blood flow and oxygenation are key. Bringing in the proper cells to heal the injured tissue and remove nociceptive stimulating chemicals can make a huge impact on the healing process.
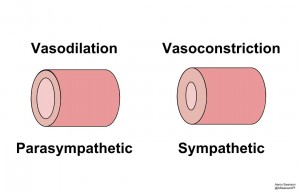
Besides the act of gas exchange, breathing affects circulation via the ANS. It does so by changing the blood vessel’s diameter: Sympathetic = Vasoconstricion (decrease diameter), Parasympathetic = Vasodilation (increase diameter). And if you remember from physics class, Poiseuille’s Equation shows that vessel diameter is one of the most important factors in determining blood flow.
It’s a four part process; you breathe more efficiently, you activate your parasympathetic nervous system, your blood vessels dilate, and you get more blood flow for growth and repair.
 3) Musculoskeletal: Provides Efficient Passive Stability for the Body
3) Musculoskeletal: Provides Efficient Passive Stability for the Body
It would be exhausting if we had to do everything volitionally with only contractile structures. Thankfully, the body has some passive stability to lighten the load (terminal knee extension, elastic recoil of tissues/tendons, foot supination for rigid osseous stability, elastic recoil of rib cage, alternating curvature of spine, etc.).
One of the more important passive stability mechanisms that we have is breathing.
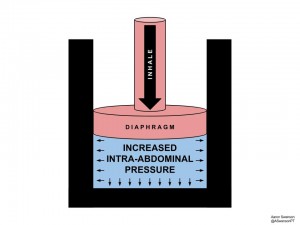
Breathing creates intra-adbominal pressure (IAP). It does this during the inhalation phase when the diaphragm compresses the intra-abdominal space like a piston. This IAP provides passive stability of the center of the body; thereby easing the muscles both proximally and distally.
By providing passive stability to the “core”of the body, the active structures are relieved, energy expenditure decreases, and compensations diminish. For example, some passive stability could relieve all those cervical muscles that are constantly trying to stabilize the head on top of the body, some passive stability could allow those paraspinals to take a much needed break, and some passive stability could provide a solid base of support so that the glenohumoral joint isn’t stuck with the bill of stability during upper extremity movements.
On the flip side of this, when the body loses this passive stability with a full exhale, it has to compensate with active stability (i.e. abdominal contraction). Clinically this can be useful to help a patient engage their abdominals or increase the difficulty of an exercise. Try having your patient fully exhale during a trunk stability exercise (e.g. bird-dog, dying bug, plank, etc.).
Summary
Understanding the affect breathing has on these 3 systems (ANS, Circulatory, Musculoskeletal) will increase one’s ability to properly prescribe breathing exercises. Improving breathing patterns can help everyone, from your athlete that gets back pain during squats to your medicare patient that has pain and stiffness when turning their head. So try giving your patients a simple breathing exercise (here and here) to help them obtain an improved nervous system, better circulation, and the power of passive stability.
References & Further Reading
Porges, Stephen W. The Polyvagal Theory: Neurophysiological Foundations of Emotions, Attachment, Communication, and Self-regulation. New York: W. W. Norton, 2011.
Courtney, Rosalba. “The Functions of Breathing and Its Dysfunctions and Their Relationship to Breathing Therapy.” International Journal of Osteopathic Medicine 12.3 (2009): 78-85.
Aaron Swanson – Breathing Part I & Part II
Physiopedia – Breathing Pattern Disorders