When a patients comes into your clinic with low back pain and you aren’t sure what is causing the pain what do you do. Should you request an x-ray?
The answer to that question is relatively simple: X-rays should only be performed in patients who have severe or progressive neurological symptoms OR suspected of having a serious underlying condition.
This is what Wang et al conclude in their new article published in the Journal of Orthopaedic Translation this month. The article is open access and a link is available below. The article provides a detailed explanation and rationale of the statement including differential diagnoses for you to consider when you are assessing patients with LBP. The table summarising these considerations is below, take a look and perhaps stick it on the wall in your office?
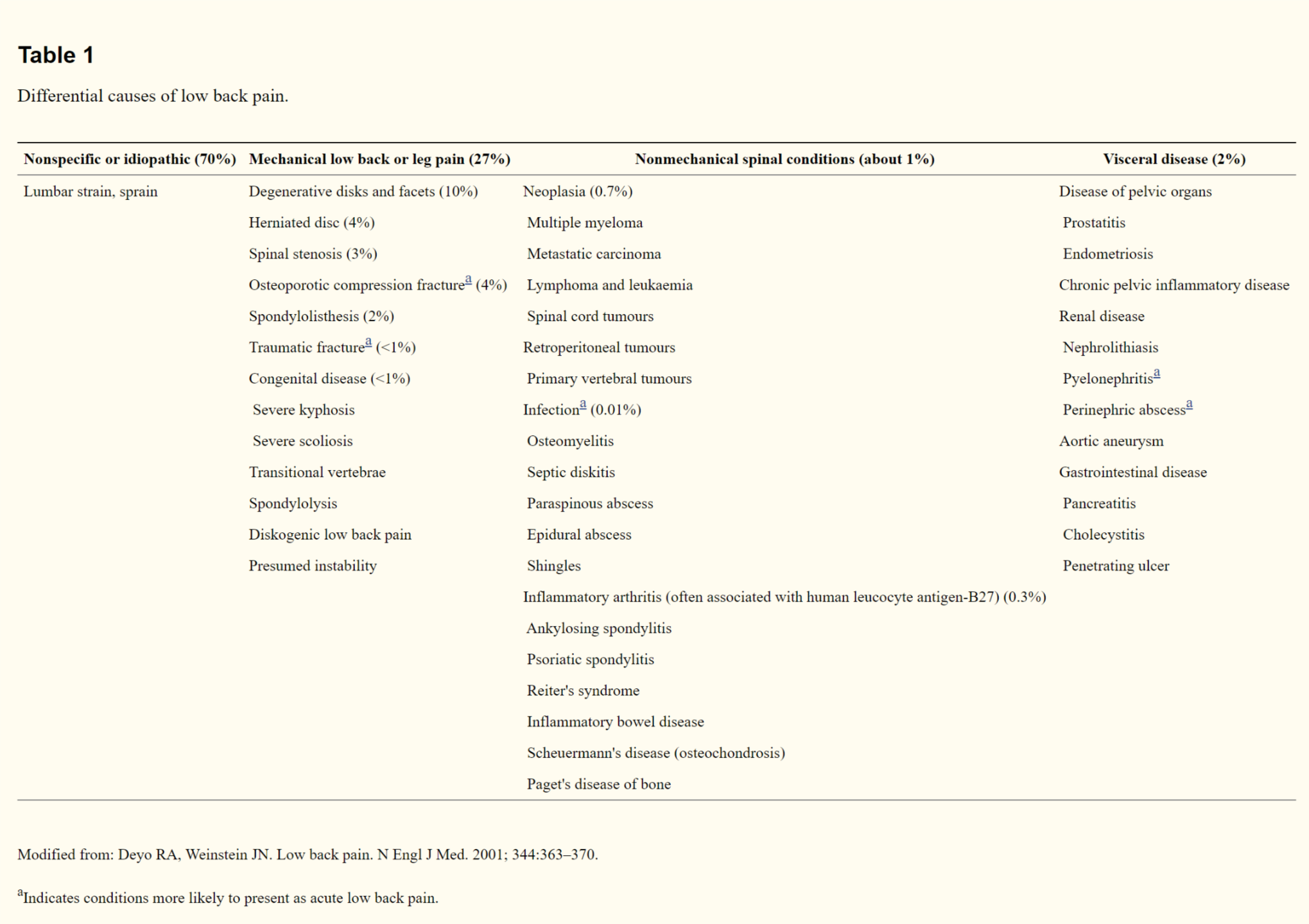
The article nicely goes through prevalence in percentages which will help understand risk and likelihood of conditions when you are in clinic so please do that the time to read through and digest what they have to say. There is one aspect of the study that is worth focusing on and that is the risks that are associated with LBP x-rays.
Potential Harms of imaging Studies for LBP
A real strength of this article is the time the authors have dedicated to explaining the costs of requesting x-rays for LBP both monetary and to the patient themselves. The monetary cost of an x-ray is relatively low at around £100 but it is what follows where the cost mounts. The imaging will likely show nothing of note and this may lead to additional tests such as bloods, follow up appointments and even MRI scans. As a meta analysis by Chou et al in the Lancet showed back in 2009 for patients without an underlying serious pathology, they gain pretty much nothing from having additional radiological investigations.
Then there is “labelling” risk that comes with x-rays. As you look at x-rays you look for any abnormality which may or may not explain their symptoms. An example being Schmorl’s Nodes which are a controversial topic as there is debate as whether these are normal variants or causes of back pain. Ultimately this is likely to hinder recovers, cause excessive worry and a cycle of fear avoidance occurs. Again this is well summarised in this article.
As you progress through your career, with the direction the profession is heading, it is entirely likely you may be put into a position where requesting x-rays is commonplace. Therefore it is important you begin to consider the implications of what you may be asked to do. This article will put you in good stead to do that.
