Blood flow restriction (BFR) training or KAATSU training, has been around for almost half a century but has recently grown into a popular mainstream strength training and rehabilitation technicque. It originated in Japan in the 1970’s by Dr Yoshiaki Sato and from it’s conception has been controversial due to the potential side effects of ecessive muscle damage and rhabdomyolysis.
The benefits of BFR are widely discussed and evidenced however there is conflicting evidence supporting different training protocols used in different populations and settings. It is also poorly understood how much muscle damage is caused by different training techniques whilst using BFR.
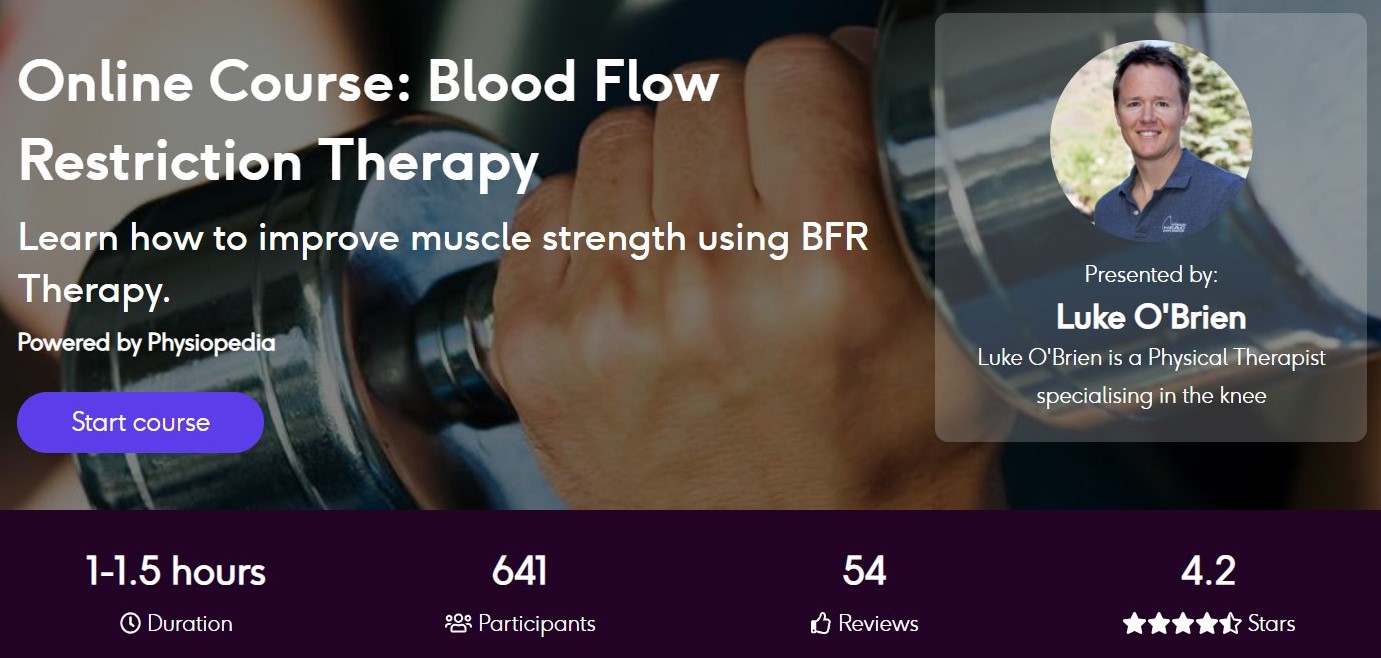
Learn to Improve Strength Safely with BFR Therapy
A new systematic review published in PLoS ONE aims to systematically analyze the evidence regarding the occurrence of muscle damage (changes in muscle damage markers) after resistance training with blood flow restriction sessions.
Methods
The systematic review followed PRISMA guidance and was pre-published in PROSPERO and adhered well to their protocol. Studies were eligible for inclusion if they were randomised or non-randomised clinical trials, published in English between 1990-2020, included humans between the ages of 18-70 and evaluated the effect with BFR using the following measures:
- DOMs
- Edema
- Inflammatory markers such as CRP
- Serum activation of muscle proteins
- ROM
- Strength
Studies involving walking, cycling, reviews, case reports and expert opinion were excluded form the analysis.
MEDLINE, PubMed, WoS, CINAHL, LILACS and SPORTdiscus were the journals selected for search using the descriptiors “resistance training” OR “strength training” AND “kaatsu” OR “vascular occlusion” OR “blood flow restriction” AND “muscle damage”. Two independent reviewers were responsible for selection of studies with a third available to reach consensus if required.
Quality of the studies included within the review was assessed using the Cochrane Risk of Bias Tool 2.0. The ROB tool was designed for use for evaluating randomised trials but was used for non-randomised trials within this study which is a clear limitation.
Analysis of Studies Included
In total 21 studies were included within the analysis which included 353 participants with an unequal reqpresentation of men (n=301) to women (n=51). The age of the participants tended to be lower and the mean ranging from 19-27 years. Study sample sizes ranged between 6-36 which indicates it’s going to be hard to draw firm conclusions form the review due to studies being under powered.
Of the studies included this is how they are broken down in terms of comparison groups:
- Ten studies compared low-load resistance training with BFR to highload resistance training.
- Nine compared resistance training with BFR to low-load resistance training.
- Three comapred eccentric to concentric in low-load training with BFR.
- Two studies compared high-load resistance training with BFR to high-load resistance training.
From an outcome measure perspective DOMs reported on a 10-VAS scale or percieved soreness during movement was the most frequently used outcome measure and used in 14 studies. The second most common was muscle edema (ten studies) which analysed cross-sectional area using MRI or USS. Muscle strength performance was also used in eight studies by using strength performance in a single joint or vertical jump force. Seven studies used ROM before and after training.
Overall the studies were of poor quality. Across the board there was inadequate reporting of randomisation with only a single study reporting how they randsomised participants. Even then participants had the freedom to choose the training session without knowledge of type of training which doesn’t sound like randomisation. Blinding was also poor across all studies so too reporting of losses during the study.
A positive is that all studies presented clear training protocols including intensity of %1RM, sets and reps, pressure applied, cuff size, recovery intervals and execution pace.
Results & Clinical Take Home
Looking at biochemical markers none of the studies demonstrated a significant increase in serum CK, LDH or Mb 24 hours after resistance training with or without blood flow restriction with low load training. However there was a significant rise in serum CK levels 24 hours after high-load resistance training with blood-flow restriction. These results should be taken with a pinch of salt however, as delayed CK elevation after moderate load training has been identified in previous studies which means we cannot exclude a delayed rise for low level training too.
This is further supported by another study included within this review which demonstrated that BFR training with low loads does increase CPK however this contrast could be explained by populations used within the study suggesting factors such as experience and duration of strength training influence physiological response to this type of training. In essence those who have trained for longer are less sensitive to a rise in CK.
The CK rise in studies which involved predetermined sessions was not high enough to cause sustained damage to the individuals. Two individuals in a study which performed reps to failure reached CK levels indicative of rhabdomyolysis which has long been a criticism of using blood-flow training.
One of the main indirect markers of muscle damage we can use if prolonged strength reduction lasting over 24 hours. Applying this to the results of this review it can be suggested that low load training with BFR does not lead to prolonged muscle damange. This is in contrast to training with high reps and volume with BFR which leads to prolonged muscle damage with the most damaging sessions being BFR with high load to muscle failure.
The results of the studies do point to a rough equivalence between BFR training at low-loads and traditional high-load training. However the study designs make it impossible to draw firm conclusions on this claim. Furthermore the addition of BFR significantly reduces the number of reps required to reach failure which can lead to misinterpretations of training volume between two groups. This is supported by the increased CK in some BFR training groups.
DOMs is one of the most commonly used measures of muscle damage in any research investigating muscle damange and BFR training is no different. Generally speaking individuals who took part in one of the studies included in this review percieved similar DOMs due to resistance training with or without blood flow restriction.
Edema was present in both BFR and traditional training groups and was not found to be significantly different between them. Post-exercise edema (<1 hr) is common and likely caused by metabolic build up, it’s unknown if the edema is different between groups.
In summary the evidence in this review suggests that the use of blood flow training at high loads of training until muscle failure lead to marked levels of muscle damage and should be avoided. BFR can also accelerate the level of fatigue and this should be reflected in protocols.
The authors of the paper summarise the use of BFR nicely:
“It is worth emphasizing that the magnitude of the muscle damage seems to be attenuated after a first session of resistance training with BFR, demonstrating a protective load effect through this type of exercise. Therefore, professionals can use a principle of progressive overload in structuring resistance training with BFR programs in clinical contexts.”