Obesity is the excessive accumulation of adipose tissue in the body due to consuming more food than is required for energy (Maguire & Haslam, 2010). BMI should be used to classify obesity (Scottish Intercollegiate Guidelines, 2011) and you are deemed obese if you have a BMI of over 30kg/m (Maguire & Haslam, 2010).
In 1980, 6% of men and 8% of women in England were deemed as obese. By 1995, these percentages had more than doubled, 15% of men and 16.5% of women were classed as obese (Anderson & Butcher, 2006). In 2010, 23.6% of men and 23.8% of women in England were obese. And the obesity levels in Scotland were slightly higher in women with 26% being obese (Maguire & Haslam, 2010). These recent statistics show that nearly a quarter of the UK adult population are obese and obesity is rising quickly, therefore it is not surprising that every year obesity in the UK costs the economy £3.5bn (Haslam, Sattar & Lean, 2007).
There are many reasons why obesity is rising rapidly, factors that we can control such as diet and exercise, and factors we can’t control, such as age, medical conditions and genetic conditions. However, I feel that the main reasons why this is happening is due to the factors we can control because they are the ones that are changing the most. People have always aged, had medical conditions and had the uncontrollable factors which could encourage obesity. But now, it has become easier to adapt to a sedentary lifestyle. I would like to discuss factors contributing to the rise in obesity levels and then progress into discussing what my role as a physiotherapist is in trying to reduce the increase.
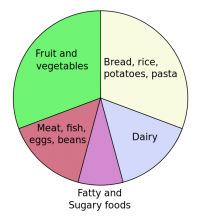
Factors such as diet play a vital role in the increase of obesity levels. Most of us know that we are meant to have a well balanced diet, every food packet shows nutritional information and the guidelines of the recommended daily amount. Regardless of this information being present, there has been a huge increase of fat content in the British diet and a diet of fats rather than carbohydrates has been thought to increase the likelihood of obesity.
In 1890, 15% of the calories consumed in the diet were derived from fat, in 1990 this had massively increased to 42% (Maguire & Haslam, 2010). This could be due to the cost of food: energy-dense foods have been found to be cheaper than fruit, whole grains and vegetables (Anderson & Butcher, 2006).
Anderson & Butcher (2006) also explains that, the portion size of a meal may contribute to obesity levels. We have seen a dramatic increase in the last half of the 1990’s, portion sizes increased more than sixty times and at the same time, childhood obesity was massively increasing. This comparison may mean that it’s not just the type of food we are eating, but how much food we are consuming. It has been argued that children will eat more, when offered larger portions (Anderson & Butcher, 2006) so maybe if portion sizes were reduced, both in readymade meals, and by parents, childhood obesity would not be as high.
I feel that schools are not sending out the right message about diet to their pupils. There have been numerous campaigns about healthy eating, such as 5 a day. However, 80% of high schools sell soda drinks, salty snacks, cakes, pastries and other foods which are unhealthy (Anderson & Butcher, 2006). Surely if these snacks were changed to fruit or a healthier option, we would see a decrease in childhood obesity. What good is it if parents are trying to give their children a healthy diet at home and the child can go to school and do the complete opposite without the parent knowing? We live in a century where food has to be quick and easily accessible quite often, be it on the way to/from work or school or when we are slightly peckish away from home. More and more people have turned to “fast food”. Processed and fast foods are associated with obesity as they contain relatively high levels of fats and carbohydrates (Maguire & Haslam, 2010).
Lastly, people may argue that a good diet depends on income. To some extent I agree with this as we have already seen that energy-dense foods are cheaper than healthier foods. On the other hand, if income levels are high, you can afford to eat out more at restaurants or have takeaways. This is a very easy and convincing option because you won’t have to spend time preparing the food and you can see how appealing this would be to a large family- quick, easy and affordable (Crawley, 2006).
The next main factor contributing to obesity is the decline in physical activity in children, young adults and adults (Lean, 1998) and this too is due to many reasons. As technology has advanced, less people have taken part in physical activity. Instead of walking to places, people drive or take the bus. This doesn’t use the energy from fat stores because it is a very short period of exercise time. Lean, Lara & O Hill, (2007) shows that a person with a normal BMI takes around 7200 steps a day, where as a person with a BMI over 30 takes around 4900 steps a day. This means that, the more times you walk to places instead of using a car may reduce the risk of obesity as more energy is being exerted. Anderson & Butcher, (2006) also shows that in 2002, 53% of parents drove their children to school and 38% used the bus. This shows that more and more people are starting to use transport more, therefore, not burning energy by walking.
Television may influence the increase in obesity, especially childhood obesity because time spent watching television could have been time spent participating in physical activity (Anderson & Butcher, 2006). A person who watches 5 or more hours of television a day takes around 5500 steps a day, where as a person who watches 0-1 hours of television a day takes between 8300 and 7800 steps a day (Lean, Lara & O Hill, 2007). This evidence proves the previous statement about television time reducing time spent exercising. Lean, ( 1998) commented that people should introduce a day where they don’t watch any television to decrease their risk of obesity. This would mean they had more spare time and could participate in exercise.
One thing I have noticed in today’s society is that gym prices are extremely high; the average price of a gym membership in my area is £25-30 a month. Depending on a person’s income this could influence their decision whether or not to buy a gym membership. The prices of sports equipment are very high too; equipment such as football boots, hockey sticks, walking boots and boxing gloves which are vital for their sports are not easily affordable. Maybe the price of sports and exercise influences participation levels.
Because obesity is reaching epidemic proportions, the topic of obesity is a core part in medical curriculums (Lean, et al 2007). This means that every time a health professional has the opportunity to see a patient, they should be able to assess the patient to see if they have a weight problem and either refer them to a specialist or offer simple advice (Lean, et al 2007). Physiotherapists have a key role to play in trying to reverse this trend as they often use exercise as a form of treatment, so if a patient is too overweight to do exercise, it becomes harder for the treatment to be successful (Bird, 1992).
From the moment a physiotherapist meets an overweight patient who can’t do the exercises required for treatment, they should express their concern about their body weight and check their BMI. If the BMI is 25 or less the physiotherapist should provide health promotion information. However if it is between 25 and 28, they should offer simple weight control advice, such as amount of calories consumed in relation to physical activity levels (Avenell, Sattar & Lean, 2007). A physiotherapist should also ask about risk factors such as smoking, excess alcohol and possibly even take blood pressure (Lean, M 1998). If the patient wants to lose weight, the physiotherapist should advise the patient to go to their doctor to devise a strategy for weight loss, which would include the help of other health professionals such as dieticians, nutritionists and behaviour therapy. On the other hand, if the patient does not want to lose weight the physiotherapist should advise them to maintain their weight and see their doctors for regular weight checks (National Institutes Of Health, 1998).
One of the main roles of a physiotherapist regarding obesity is educating patients. Bird, (1992) states that many people are falsely led to believe that they can lose weight without putting in effort or changing from a sedentary lifestyle. Physiotherapists have to explain why that is not true, because if the patient doesn’t understand why this is incorrect, they will continue to believe it. Health professionals should encourage healthy eating, consisting on the 5 food types, information can be given to patients via the “eatwell plate” model (Scottish Intercollegiate Guidelines, 2011). However, what good is offering this advice if health professionals don’t follow it? Physiotherapists should therefore “practice what they preach” and follow a healthy diet themselves (Lean, 1998).
We should also make patients aware of the numerous benefits of modest weight loss (Scottish Intercollegiate Guidelines, 2011) benefits such as reduced risk of cancer and diabetes but also the holistic benefit of having an improved physical, social and mental well being.
One of the most important things a physiotherapist must take into consideration is that they “should be appropriately trained and qualified to deliver the specific interventions and have ongoing specialist supervision where relevant” (Scottish Intercollegiate Guidelines, 2011). If they don’t, they are liable to be questioned as they may have given out incorrect information. Physiotherapists are not responsible for setting goals or weight management programmes, therefore it is vital that they understand the importance of referral to a specialist.
Lastly, physiotherapists should make patients aware about when they are more likely to put on weight, for example, pregnancy or the menopause so that the patient can prepare for it or at least not be surprised if it does happen. Lean, et al, (2007) suggests that health professionals should get involved with the food industry and the environment in order to try and promote physical activity, healthy eating and better self confidence. This would be extremely difficult to do because fast food companies are making their products for a profit, not for health issues. What they are doing now is making them a huge profit so why would they try to change when they are being very successful?
The main message from this discussion is that although obesity levels are rising extremely quick due to a number of factors, health professionals such as physiotherapists should be able to recognise obesity, advise a patient on diet and physical activity and be able to refer them for further advice or treatment to do with their body weight. This should hopefully make more people aware of the increasing problem but also, help to reduce the levels of obesity and reduce levels of problems caused by obesity.
References
- Anderson, P & Butcher, K (2006) Childhood Obesity: Trends and Potential Causes, The Future of Children, 16 (1) Princeton University and The Brookings Institution.
- Crawley, J (2006) Markets and Childhood Obesity Policy, The Future of Children, 16 (1) Princeton University and The Brookings Institution.
- Haslam, D, Sattar, N & Lean, M (2007) Obesity- time to wake up. In: Sattar, N & Lean, M (eds.) ABC of Obesity. Oxford, Blackwell Publishing.
- Maguire, T & Haslam, D (2010) The Obesity Epidemic and Its Management [Online] London. Pharmaceutical Press. Available fromhttp://lib.myilibrary.com/Open.aspx?id=239868&src=0 [Accessed 6/3/2012]
- Avenell, A, Sattar, N & Lean, M (2007) Management: Part I- Behaviour change, diet and activity. In Sattar, N & Lean, M (eds.) ABC of Obesity. Oxford, Blackwell Publishing.
- Lean, M, & Lara, J & O Hill, J (2007) Strategies for preventing obesity. In: Sattar, N & Lean, M (eds.) ABC of Obesity. Oxford, Blackwell Publishing.
- Lean, M. et al (2007) Obesity- can we turn the tide? In: Sattar, N & Lean, M (eds.) ABC of Obesity. Oxford, Blackwell Publishing.
- Lean, M (1998) Clinical Handbook of Weight Management. London. Martin Dunitz Ltd.
- National Institutes Of Health (1998) Clinical Guidelines On The Identification, Evaluation And Treatment Of Overweight And Obesity In Adults-The Evidence Report. NIH Publication No. 98-4083.
- Bird, S (1992) Exercise Physiology For Health Professionals. London. Chapman & Hall.
- Scottish Intercollegiate Guidelines (2011)Management Of Obesity- Quick Reference Guide. [Online] Edinburgh. Scottish Intercollegiate Guidelines Network. Available from http://www.sign.ac.uk/pdf/qrg115.pdf [Accessed 13/3/2012]