Rehabilitation 2030 established the need to strengthen and integrate rehabilitation professions into health systems around the world. Unfortunately, limited opportunities in entry-level education and continuing professional development across all rehabilitation professions has impacted workforce capacity, especially in low-resourced areas. The focused symposium “Leveraging collaborative inter-professional education strategies for context-specific workforce development” at the recent World Physiotherapy Congress was an opportunity to discuss this topic in detail and showcase experiences from several different contexts.
Imagine a world where there was an abundance of rehabilitation providers that were equipped with up-to-date, evidence-informed, and competency-based education. Even more so, visualise a place where rehabilitation providers learned and worked alongside each other in the classroom and in clinical practice, sharing knowledge and resources, drawing upon the distinctive skills connected with their unique professions in person-centered care.
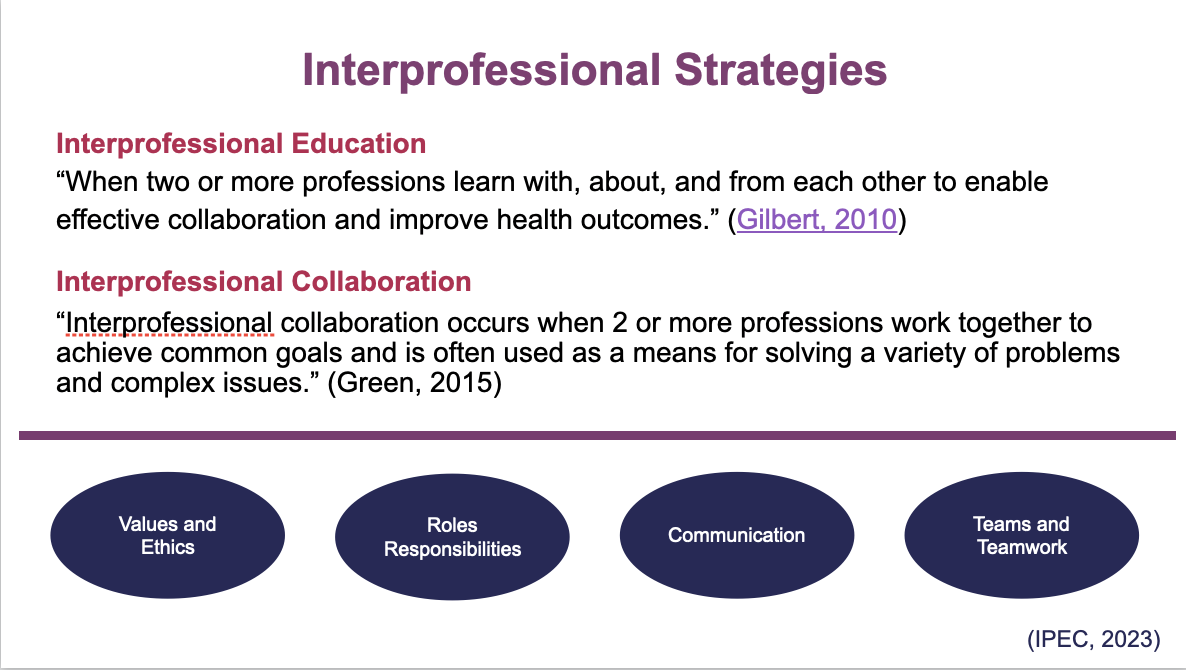
The benefits of interprofessional collaboration include improving the ability to educate more providers with limited human resources, increasing the awareness of individual professions within rehabilitation and also across the wider health system. A key step in making this vision a reality is to understand the education, competency, and practice expectations for each profession and to draw upon commonalities and appreciate differences.
The research presented by Cheryl Footer in this focused symposium built on the findings from a situation analysis of current global rehabilitation education, which identified a significant gap in education and regulation of the rehabilitation professions, especially in low- and low-middle income countries. An international and interprofessional rehabilitation team developed a framework to review, compare, and contrast regulation and education strategies and expectations across rehabilitation professions internationally. The process was informed by survey data, interview data, and a review of more than 200 documents including standards of practice, standards of education, professional competencies, curricular plans, and course syllabi. The mapping exercise provided an understanding of similarities and differences within and between professions and global regions, and to identify opportunities for collaboration.
An International Rehabilitation Education and Training Toolkit is being developed as a result of this work. The toolkit, which encourages interprofessional collaboration, includes tools that guide stakeholder organisations to reflect on national professional regulation strategies, academic programs and clinical training opportunities. The toolkit was then implemented as appropriate in four countries: Myanmar, Ukraine, Uganda, and Pakistan. Neelum Zehra (Occupational therapist, Pakistan), Olha Kovalchuk (Ministry of Health, Ukraine), Herbert Omoding (Physiotherapist, Uganda) and Hsu Wai Mon Oo (Physiotherapist,Myanmar) shared perspectives of the toolkit implementation, providing additional insights into interprofessional strategies for strengthening the rehabilitation workforce..
The research, toolkit and experiences presented show that through international and interprofessional collaboration it is possible to identify best practices and gaps that can provide a solid foundation for developing policy, curricula and training opportunities, achieving resource efficiencies, and for creating relevant and informed workforce development strategies that meet local expectations for standards of practice and competencies in rehabilitation provision.

This work is supported by the USAID funded Learning Acting Building for Rehabilitation in Health Systems (ReLAB-HS) project and is not possible without the generous and committed contribution of the Leahy War Victims fund. ReLAB-HS is made possible by the generous support of the American people through the United States Agency for International Development (USAID) and
is implemented under cooperative agreement number 7200AA20CA00033. The consortium is managed by prime recipient, Johns Hopkins Bloomberg School of Public Health.