Accurately identify the wide-ranging, systemic effects of spondyloarthropathy is key to enabling early diagnosis.
For many rheumatology conditions there are considerable delays to diagnosis. These delays consequently affect accurate, timely treatment, subsequent intervention and, most importantly, impact the quality of life of the people living with these burdensome conditions. The British Society for Rheumatology (BSR, 2015) published a policy report outlining key challenges and opportunities facing rheumatology services in the United Kingdom. They highlighted the importance of early diagnosis and proposed a ‘12-week window of opportunity’ in which to positively affect patient care by referring appropriately to a rheumatologist within this time.
Moreover, a national clinical audit for rheumatoid arthritis and early inflammatory arthritis which aimed to assess the early management of patients referred to rheumatology providers with suspected inflammatory arthritis within England and Wales. The audit confirmed that most people with early inflammatory arthritis wait too long from when their symptoms start to when they start disease-modifying treatment. The audit also found that there were often delays in referral from GPs and then further delays following their initial referral. I would go further to infer that delays also happen within the settings of physiotherapy practice too.
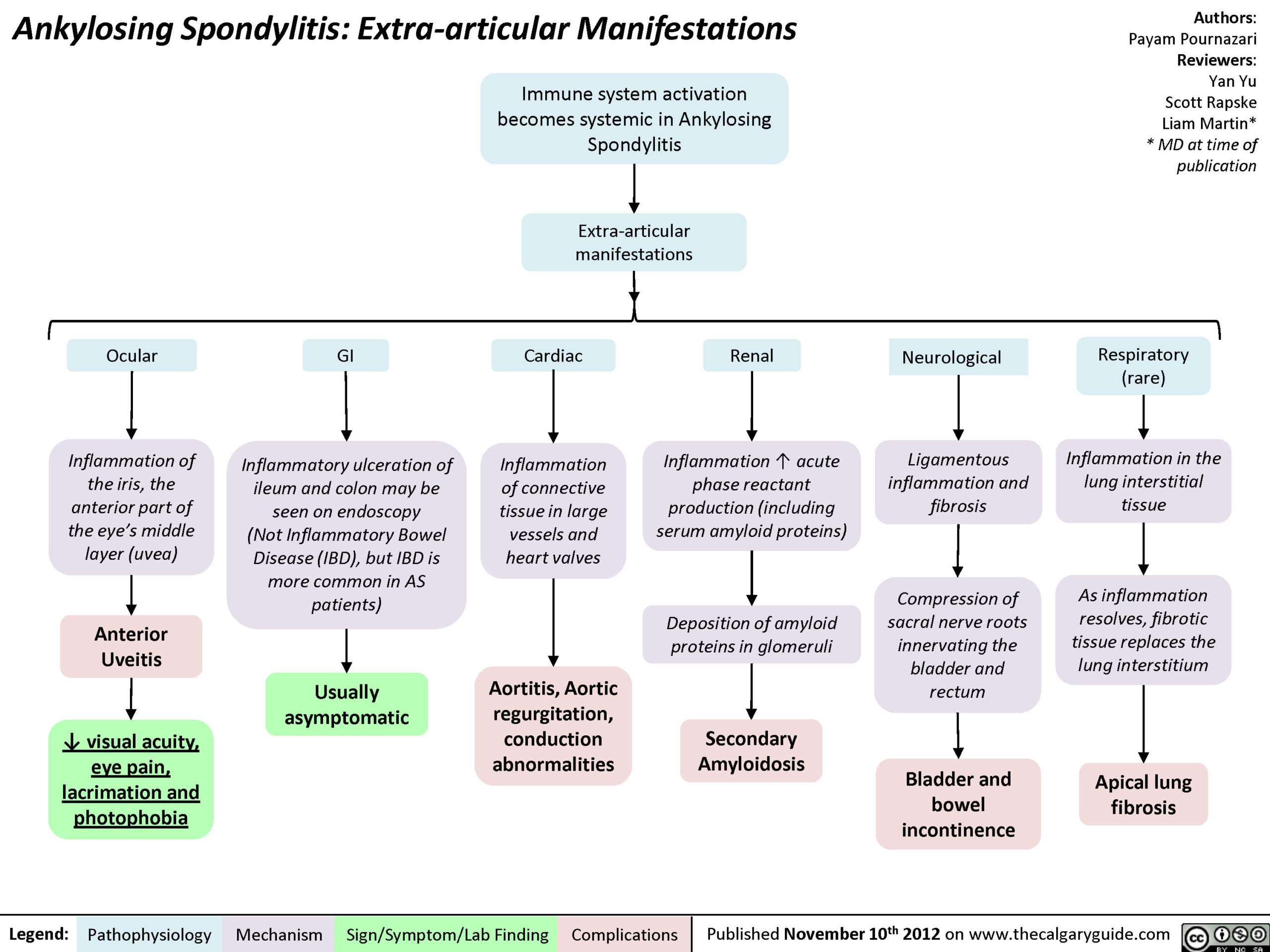
Generally, intra-articular features suspicious of synovitis and systemic inflammation are clear cut and frequently noted; the cardinal signs of inflammation for example (erythema, heat, oedema), along with pain, stiffness, and restricted range of motion. Extra-articular manifestations (EAMs), those situated or occurring outside of a joint, however, are often less well known.
Extra-Articular Manifestations are Key to Early Diagnosis
Furthermore, these EAMs prove particularly elusive if:
- Symptoms are palindromic (flare and don’t return for some time)
- Symptoms mimic musculoskeletal conditions or merge between several rheumatic disorders unnoticed
- Patients are unable to identify symptoms as being related to rheumatology
- There is a low index of suspicion for systemic inflammatory conditions
It’s easy to see then, why there are lengthy delays to diagnosis in some of these conditions. The delay is still around eight years in some conditions like Axial Spondyloarthritis (axSpa, previously known as Ankylosing Spondylitis, AS) and we could do a lot to help change this.
Physiotherapists have the opportunity to think there’s a possibility, spot the signs and quickly refer into the appropriate pathway for the benefit of the patient, in line with current guidance.
But where to start? I suggest the following:
- Build an awareness of rheumatology conditions
- Develop your inflammatory pattern recognition
- Take note of Extra-Articular Manifestations
Awareness of Rheumatology Conditions
 Including a possible inflammatory diagnosis or differential diagnosis can be the mark of a holistic, vigilant and alert clinician. Similarly, like with other systems such as vascular or neurologic, a high index of suspicion is justified.
Including a possible inflammatory diagnosis or differential diagnosis can be the mark of a holistic, vigilant and alert clinician. Similarly, like with other systems such as vascular or neurologic, a high index of suspicion is justified.
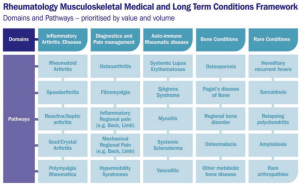
There are over 200 rheumatic and musculoskeletal disorders and in terms of volumes of patients with the condition, or cost of interventions, the table below is a guide to the main conditions out there.
Inflammatory Pattern Recognition
An inflammatory pattern may be stand-alone from your initial assessment, mixed with other presentations or indeed become more apparent in subsequent patient sessions.
Below are some key pointers towards a potentially inflammatory pattern:
- Insidious onset
- Morning joint or back stiffness >60mins, usually lasting a few hours
- Symptoms settle with moderate activity and become worse with rest (often paradoxical to a ‘mechanical’ pattern)
- Night pain
- Family history of rheumatoid conditions
- Onset < 45 years of age (can be younger in axSpa, 20s – 30s)
- Good response to non-steroidal anti-inflammatory medications
Additionally, here are those often more pertinent to spondyloarthropathy:
- Chronic inflammatory back pain (>3 months)
- Human Leukocyte Antigens B27 (HLA-B27) gene positive
- Raised inflammatory markers – CRP & ESR
- Presence of spinal inflammation in early and active disease best viewed on MRI change
Extra-Articular Manifestations
As mentioned previously, it important to be aware of EAMs and the common signs or coexisting pathologies linked to rheumatology conditions. A recent study in people with rheumatoid arthritis found that 27% of patients had extra-articular manifestations. Further still, Pieren et al (2016) found that more than half of 394 patients with spondyloarthritis had extra-articular manifestation, among the most frequent of those were psoriasis and uveitis.
The following are common EAMs to watch out for:
- Psoriasis plaques / rashes
- May be associated with Psoriatic arthritis or spondyloarthropathy
- Inflammatory Bowel Disease (or history of IBD)
- Including Crohn’s disease, Coeliac disease and Ulcerative colitis, may suggest spondyloarthropathy
- Anterior uveitis (or Iritis)
- Eye inflammation may be present in reactive arthritis or axSpa
- Inflammation of entheses
- Insertional Achilles tendinopathy, plantar fasciopathy, patella tendinopathy for example
- Disorders of the attachment of tendon or ligament to bone (enthesis) are common in a number of conditions
- Nail abnormalities (such as koilonychia and onycholysis)
- Present in psoriatic arthritis and systemic lupus erythematous
- Dactylitis of digits
- ‘Sausage digits’ common in psoriatic arthritis
- Rheumatoid Nodules
- More common in rheumatoid arthritis
- Purpura spots
- (evident in Henoch Schloein purpura disease)
- Interstitial lung disease
- Anaemia
- Keratoderma blennorrhagica rash
- Most often seen in reactive arthritis
- Dry eyes (and mouth)
- Common symptoms of Sjogren’s Syndrome and often associated with rheumatoid arthritis
Summary and Key Take Homes
Patients with inflammatory musculoskeletal conditions frequently present to physiotherapists in a number of settings, masquerading as a ‘mechanical’ condition. For me, the exciting aspect of our role is deciphering these cloaked symptoms, considering if there truly is a rheumatology element at hand. By being more vigilant of rheumatology conditions and both their intra- and extra-articular manifestations, we as clinicians are in line with current evidence and best practice.
Intra- and extra-articular manifestations are clues to systemic inflammatory aetiology, but we must of course be careful. We risk inundating our medical colleagues with requests to consider our suspicions; an insertional achilles tendinopathy can easily be mistaken for a rheumatology-related enthesopathy.
Nevertheless, in my opinion, we must continue to be suspicious. If we are successfully having the thoughts and discussions, we as physiotherapists are able to help shift the direction of care for people with rheumatology conditions and will continue to advance timely, accurate diagnosis, treatment and management.
This post was originally published June, 2017 and written by Chris Martey. The page has now been updated for freshness, accuracy and comprehensiveness.
References
British Society for Rheumatology (2015) The State of Play in UK Rheumatology: Insights into service pressures and solutions. [Accessed 11th May 2017 https://www.rheumatology.org.uk/Portals/0/Policy/Policy%20Report/Rheumatology%20in%20the%20UK%20the%20state%20of%20play.pdf].
British Society for Rheumatology (2016) National Clinical Audit for Rheumatoid and Early Inflammatory Arthritis: a patient and public guide. [Accessed 11th May 2017 https://www.rheumatology.org.uk/Portals/0/Policy/Audit%20reports/Patient%20guide%20-%20national%20clinical%20audit%20for%20rheumatoid%20and%20early%20inflammatory%20arthritis%20-%20second%20report.pdf]
Brukner, P., & Khan, K. (2012) Clinical Sports Medicine. 4th ed, McGraw-Hill Australia Pty Ltd. Australia.
Kalappan, M., Abubacker, N.R.T., Shetty, M., Rajendran, K., Rathinam, W.K.M. and Karuthodiyil, R., 2017. Study of extra-articular manifestations and disease severity in patients with rheumatoid arthritis. International Journal of Advances in Medicine, 3(1), pp.53-56.
Ledingham, J.M., Snowden, N., Rivett, A., Galloway, J., Ide, Z., Firth, J., MacPhie, E., Kandala, N., Dennison, E.M. and Rowe, I., 2017. Achievement of NICE quality standards for patients with new presentation of inflammatory arthritis: observations from the National Clinical Audit for Rheumatoid and Early Inflammatory Arthritis. Rheumatology, 56(2), pp.223-230.
Pieren, A., Peiteado, D., de Miguel, E., Espinel, M., Moral, E., Monjo, I., Paredes, M.B., Tornero, C., Bonilla, G., Plasencia, C. and Nuño, L., 2016. FRI0405 Extraarticular Manifestations in Patients with Spondyloarthritis under Biologic Treatment. Annals of the Rheumatic Diseases, 75(Suppl 2), pp.582-582.
Siegel, E.L., Orbai, A.M. and Ritchlin, C.T., 2015. Targeting extra-articular manifestations in PsA: a closer look at enthesitis and dactylitis. Current opinion in rheumatology, 27(2), pp.111-117.
Singal, A. and Arora, R., 2015. Nail as a window of systemic diseases. Indian dermatology online journal, 6(2), p.67.
Stolwijk C, van Tubergen A, Castillo-Ortiz JD. (2015) Prevalence of extra-articular manifestations in patients with ankylosing spondylitis: a systematic review and meta-analysis Annals of the Rheumatic Diseases;74:65-73.
Websites [accessed May 2017]:www.arthritisresearchuk; www.nass.co.uk; www.rheumatology.org.uk