I was recently in a community round table discussion on what we do with lateral epicondyle patients. It was led and moderated by a physician, who I was excited to hear no longer injects these patients with cortisone. The re-occurrence rates are incredibly high after an injection and the potential for a worse outcome due to weakening the tendon tissue is too great.1 I applauded his change in practice to help his patients! The conversation continued on and PTs in the room weighed in on how they treat these patients. “I massage them.” “I do core strengthening with them.” “I work on their rotator cuffs.”
I waited and waited, but no one presented the solution all rehab professionals should be stating. “I am guided by the best available research and use my clinical reasoning to further adapt my plan to my patient.” In the past, I have written about the need for us to adapt to individual patients based on both our understanding of the clinical and personal problem!
So, what does this mean for lateral epicondyle pain? Let’s dive into this a bit and explore the problems and potentials. When you dive into randomized trials, you will find only mild influences of PT intervention. I believe this is due to 2 specific reasons:
- Most lateral epicondyle patients improve within 1 year, so 1 year follow-ups are difficult to get significant differences no matter the interventions.1
- Lateral epicondyle pain is not a homogenous group.4 To perform a Randomized Control Trial (RCT), you typically try to control for all variables and only adjust 1 specific parameter, which is your treatment intervention.
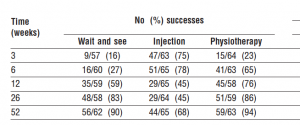
Let’s explore the first issue first. This was illustrated perfectly, with a large number of patients by Bisset et al 20061 (Table Below). You’ll see that 90% of those who did not receive treatment were better at 1 year. From a research standpoint, this would indicate that I should just wait, but what if it were you personally? What if you were complaining of lateral elbow pain for a year? Do you want to wait 1 year or do you want a solution now? Maybe I differ from the crowd, but if I could have a substantially better chance of being better within 1 or 2 months, I’m taking that route.
So this data establishes that most lateral epicondyle patients do get better and our 1 year outcomes are difficult to compare because most get better eventually no matter the treatment. That doesn’t address the RCT issue though. When you look at a Meta-analysis2, you will walk away a bit disheartened, thinking, well what do I do now? The evidence is murky and doesn’t point us towards a clear treatment. This is nothing new in the PT world.
If you treat the lumbar spine, hopefully you are not treating every low back pain patient the same. For years, we weren’t sure if manipulation helped, but then Tim Flynn came along and published a Clinical Prediction Rule to help us identify who to manipulate.5 The pain science researchers are now guiding us on who and how to deliver interventions to low back pain with a contribution from a complex origin. We have discovered that low back pain is not a homogenous group and if we deliver only one intervention to a broader population, then there is a diluting effect that causes it to look like nothing is effective.
This brings us back to the issue with lateral epicondyle pain. At the heart of it, this is a painful experience due to the inability to tolerate load at the tendon. However, we need to dive deeper to determine why the tendon can’t tolerate the load and that is where our issues as a rehabilitation profession often go awry. Let’s list out some reasons the tendon can’t tolerate the load:
- The tendon can’t tolerate the load because of the muscle/tendon strength. We could go into this deeper and discuss actual specific tissue changes, but for now, let’s just keep this as it needs to be loaded. This behaves similar to the literature for patella tendon and Achilles tendon and needs to be progressively loaded.
- The tendon is being overloaded due to a rapid increase in activity. In the short-term, this tendon needs to have load reduced. This person should use a brace, taping, or some other means of reducing the load.
- The tendon is not tolerating the load from a contribution of a psychosocial or centrally sensitized phenomena and we need to intervene from a behavioral and mindset perspective.4
- The tendon is not tolerating the load with a cervical influence, whether a referral, radiculopathy, or just something we don’t completely understand with afferent and efferent signaling. This responds well to the addition of cervical treatment.3
- The tendon is not tolerating the load because of a local joint issue, whether humeroulnar or radial head in nature. This responds well to adding mobilizations.1
- The tendon is not tolerating the load because of a hypomobile carpal issue, resulting in greater requirements of the wrist extensors to overcome the hypomobility during function. This responds well to adding carpal mobilizations.6
- A combination of two or more of these factors.
When we look at lateral epicondyle pain from a perspective of these 7 issues, we can start to see that unless we design studies which allow the clinician to alter the course of treatment based on the impairment driving the problem, then our results will be diluted in publications. The alternative would be to recruit thousands of patients in order to power a study (or studies) large enough to allow each of these patient populations to be placed in their own group and delivered a more specified intervention. Still, it is my experience that most lateral elbow pain patients have at least 2 of these issues, and many have a multitude of impairments. As clinicians, we should look at that as an advantage. The more things which are not working efficiently, the more opportunities we have to help our patients.
Looking for more Tips, Tricks, and Rehab Ideas? Follow Me On Twitter
References
- Bisset L, Beller E, Jull G, Brooks P, Darnell R, Vicenzino B. Mobilisation with movement and exercise, corticosteroid injection, or wait and see for tennis elbow: randomized trial. BMJ. 2006;333(7575):939-944.
- Bisset L, Paungmali A, Vicenzino B, Beller E. A systematic review and meta-analysis of clinical trials on physical interventions for lateral epicondylalgia. B J Sports Med. 2005;39:411-422.
- Cleland JA, Whitman JM, Fritz JM. Effectiveness of manual physical therapy to the cervical spine in the management of lateral epicondylalgia: A retrospective analysis. J Orthop Sports Phys Ther. 2004;34:713-724.
- Coombes BK, Bisset L, Vicenzino B. Management of lateral elbow tendinopathy: One size does not fit all. J Orthop Sports Phys Ther.
- Flynn T, Fritz J, Whitman J, et al. A clinical prediction rule for classifying patients with low back pain who demonstrate short-term improvement with spinal manipulation. Spine. 2002;27:2835.
- Struijs PAA, Damen PJ, Bakker EWP, Blankevort L, Assendelft WJJ, van Dijk, CN. Manipulation of the wrist for management of lateral epicondylitis: A randomized pilot study. Physical Therapy. 2003;83(7):608-616.