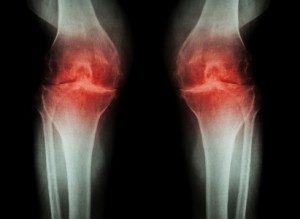
There are approximately 100 different types of known arthritis, with the two most well-known being osteoarthritis (OA) and rheumatoid arthritis (RA).
OA is the most common form of arthritis which, although can be affect people of any age, sees a steady increase in prevalence with age. OA typically involves inflammation and structural changes of the joint, causing pain, functional disability and reduced quality of life (Cross et al, 2014). Arthritis Research UK (2014) highlight that approximately 8.75 million people have sought treatment for OA with just over half having knee OA.
RA is an autoimmune inflammatory arthritis that, like OA, has a significant impact on the ability to perform daily activities, health-related quality of life due to structural changes that occur as a result (Singh et al, 2016).
The World Health Organisation, in conjunction with the American College of Sports Medicine provided recommendations for physical activity levels in health adults which has been widely recognised and promoted. Part of these recommendations is that:
‘Healthy adults aged 18-65 years should participate in moderate intensity aerobic physical activity for a minimum of 30 minutes 5 days per week or vigorous intensity aerobic activity for a minimum of 20 minutes 3 days per week’
While evidence, such as the systematic review by Fransen in 2015, highlights the positive impact of physical activity, people with rheumatic and musculoskeletal diseases are generally less active compared to healthy controls while type and dosage of exercise still remain unclear.
To address this, a EULAR task force was created to:
- Evaluate if the physical activity recommendations are applicable to inflammatory arthritis and OA
- Develop evidence based recommendations on physical activity promotion and delivery in the management of people with inflammatory arthritis and OA.
- Formulate an educational and research agenda.
In this paper, inflammatory arthritis encompasses RA and Spondyloarthritis while OA encompasses hip and knee OA.
22 European experts formed the multidisciplinary task force ranging from medical doctors to human movement scientists plus 3 patient representatives. Two systematic literature reviews were performed; one to investigate the effectiveness, safety and feasibility of physical activity while the other investigated facilitators and barriers towards physical activity.
The results from the systematic literature review were presented during the second meeting of the task force, allowing the experts to draft 10 recommendations through discussion and consensus. After the second meeting, the recommendations were sent to members of the task force via email to allow them to rate the level of agreement for each.
Clinical Considerations
The literature search resulted in 96 papers from which 4 overarching principles and 10 recommendations for physical activity based on these results and expert opinion were produced. The recommendations are as follows:
- Promoting physical activity consistent with public health physical activity recommendations should be an integral part of standard of care throughout the course of disease.
- All health care providers should take responsibility for promoting physical activity and making necessary referrals to make sure the receive the appropriate physical activity interventions.
- Physical activity should be delivered by health care providers component in their delivery.
- Health care providers should evaluate peoples current physical activity levels to identify which areas require improvement.
- General and disease-specific contraindications for physical activity should be identified and taken into account in the promotion of physical activity
- Physical activity interventions should have clear personalised aims that should be evaluated by the use of subjective and objective measures.
- General and disease specific barriers and facilitators related to performing physical activity should be identified and addressed.
- Where individual adaptations to general physical activity recommendations are needed, these should be based on comprehensive assessment of physical, social and psychological factors including fatigue, pain, depression and disease activity.
- Health care providers should plan and deliver physical activity interventions that include behavioural change techniques.
- Healthcare providers should consider different modes of delivery of physical activity in line with people’s preferences.
Conclusion
The results from this task force correlates with previous research that exercise is beneficial to those with both inflammatory and osteoarthrosis. However, the paper does highlight that physical activity promotion is a behavioural intervention and should therefore form a key part in physical activity interventions.
Although a literature review formed a key part in the formation of the recommendations, there was only one reviewer of the abstracts with a second person involved in screening unclear abstracts which doesn’t comply with the standard procedures for producing systematic literature reviews.
Also, while the paper addresses the most prevalent inflammatory and osteoarthritic conditions, large heterogeneity between conditions may limit the precision of the recommendations and sub conditions, such as juvenile arthritis, were not considered.
Exercise continues to demonstrate its usefulness in improving the outcomes and quality of life in a large majority of conditions. However, as physiotherapists we need to understand the individual barriers that a person may hold against physical activity, address them empathically, utilise behavioural change techniques such as education and work collaboratively with our patients to implement a graded programme to achieve the public health physical activity guidelines on physical activity.
References
- Arthritis Research UK (2014). Arthritis in the UK – Facts and Statistics. Available at: https://www.arthritisresearchuk.org/~/media/Files/Arthritis-information/Arthritis%20key%20facts.ashx arthritis research UK facts and figures [Accessed 3rd November 2018].
- Cross, M., Smith, E., Hoy, D., Nolte, S., Ackerman, I., Fransen, M., Bridgett, L., Williams, S., Guillemin, F., Hill, C.L. and Laslett, L.L. (2014). The global burden of hip and knee osteoarthritis: estimates from the global burden of disease 2010 study. Annals of the rheumatic diseases, 73(7), pp.1323-1330.
- Fransen, M., McConnell, S., Harmer, A.R., Van der Esch, M., Simic, M. and Bennell, K.L. (2015). Exercise for osteoarthritis of the knee: a Cochrane systematic review. Br J Sports Med, pp.bjsports-2015.
- Garber, C.E., Blissmer, B., Deschenes, M.R., Franklin, B.A., Lamonte, M.J., Lee, I.M., Nieman, D.C. and Swain, D.P. (2011). Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Medicine & Science in Sports & Exercise, 43(7), pp.1334-1359.
- Singh, J.A., Saag, K.G., Bridges Jr, S.L., Akl, E.A., Bannuru, R.R., Sullivan, M.C., Vaysbrot, E., McNaughton, C., Osani, M., Shmerling, R.H. and Curtis, J.R. (2016). 2015 American College of Rheumatology guideline for the treatment of rheumatoid arthritis. Arthritis & rheumatology, 68(1), pp.1-26.