Hello to all and welcome to my blog courtesy of stopsbackpain.com.au.
Today we’re going to talk about psychosocial factors.
Back when I graduated from physiotherapy in 1988 psychosocial factors were not often discussed in reference to low back pain. Even in 2000 when I commenced my PhD, I struggled to find a physiotherapy supervisor who was willing to countenance a thesis that included both pathoanatomical and psychosocial factors.
My how times have changed! Social media, the popular press and scientific journals are full of information encouraging the use of psychosocial factors in assessment and in assessment and treatment of low back pain. So much so that some authorities, including our own group(Ford and Hahne 2013), have suggested that the pendulum has swung too far.(Jull and Moore 2012) Assumptions around relative importance of psychosocial factors over pathoanatomical factors in low back pain is not supported by a recent systematic review showing the amount of variance in outcome explained by psychosocial factors to be less than 25%.(Wessels et al., 2006).
Nevertheless, there is substantial evidence suggesting that psychosocial factors should form part of a balanced approach to patient management within the context of a biopsychosocial model. How should this work?
Rule number 1 – Don’t persist with physical based treatment without assessing psychosocial factors in patients not progressing
It’s surprising how many cases I see where practitioners persist with manual therapy or soft tissue work without formally assessing psychosocial factors despite the patient not improving. Whilst psychosocial factors are not the be all and end all, the evidence is clear that in patients not improving with standard treatment these “yellow flags” need to be assessed.(Dagenais, Tricco et al. 2010)
It is also quite common to see a practitioner using a psychosocial screening tool such as the Örebro Musculoskeletal Pain Questionnaire or STarT Back tool, without actually using the results to direct treatment. Some practitioners also use the Örebro as an outcome measure rather than its intended purpose of identifying patients at risk of poor outcome and modifying treatment accordingly.
Screening tools for psychosocial factors seem to be more commonly used in patients with a compensable injury. Perhaps this is due to pressure from third party payers? Yet psychosocial factors are equally important in private patients and should be assessed when appropriate. I’ve had many private patients with major psychosocial issues that wouldn’t have been revealed unless further assessment was undertaken. Commonly these patients burst into tears on the introductory question!
If your patient is not responding to physical based treatment after 5-8 sessions you should provide them with a psychosocial screening tool questionnaire. Provided a reasonable explanation is given to the patient they should happily fill this in. See my free eLearning module on screening tools here.
Rule number 2 – Further explore the results of your psychosocial screening tools
When using screening tools it is important not to stop at the overall score. A score of 130/210 for the Örebro or a “high risk” rating for the STarT Back tool indicates that psychosocial factors are likely to be relevant. However, looking at scores on individual items from these questionnaires provides valuable additional information. The Örebro is heavily influenced by activity limitation (eg walking/shopping) due to 5 specific items. Consider the difference in management for a patient who scores:
- 10/10 on the Örebro anxiety and depression items and an average of 5/10 on the activity limitation items
- 2/10 on the Örebro anxiety and depression items and an average of 9/10 on the activity limitation items
The second patient may well have severe pathology causing the activity limitation in the absence of significant psychosocial factors, whereas the first is likely to require psychological and/or medical intervention.
Practitioners should also consider further exploring the individual items with specific questions using the principles of “narrative reasoning” which have been well described.(Jones and Rivett 2004) Future blogs will focus on this in more detail.
Rule number 3 – Triage your patient’s treatment based on your findings
As already stated, there is no point in using screening tools if it doesn’t change your treatment plan. There comes a time with manual techniques where if a change isn’t occurring, the treatment approach should be modified. What is “clinically important change”? Well that in itself is a complex question, but Maitland reassesses patients every 6 sessions or so and if there is no compelling evidence (using standardised outcome measures, pain, and patient specific measures) of sustained improvement. Depending on the results of that assessment, consideration of other approaches should then be given. In these patients where change is not occurring, some key markers indicating the need to change tack include:
- Örebro over 130/210 – unless unduly influenced by severe pathology strong consideration should be given to changing approach addressing specific barriers to recovery
- Depression score on Örebro over 8/10 indicating the need for further assessment and probably management via a psychologist and/or medical doctor
- Multiple work items on Örebro over 8/10 indicating the need for contact with the worksite and possible worksite assessment ± engagement with other stakeholders (insurer, occupational rehabilitation provider)
- Örebro over 150/210 indicating a high risk of poor outcome with a multidisciplinary pain management assessment (including a pain physician, psychologist and usually physiotherapist) the most effective path to identifying barriers to recovery and a suitable management plan
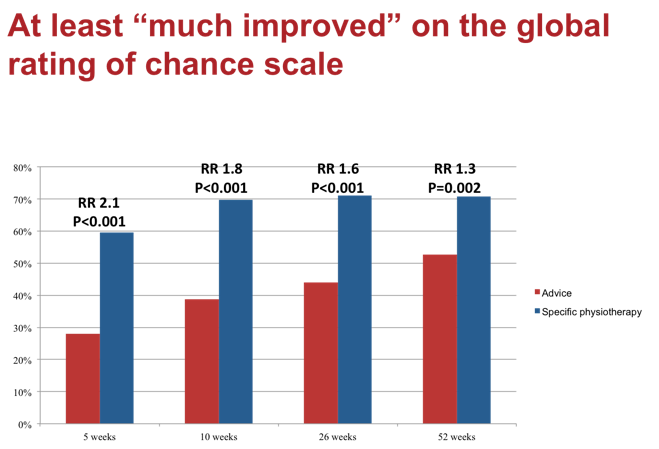
Our recently completed randomised controlled trial (Specific Treatment of Problems of the Spine – STOPS) used the Örebro in subgrouping and clinical decision making. The results will be published soon, however some of the data are presented below. We believe our results show compelling information supporting stratified physiotherapy based on an accurate interpretation of the biopsychosocial model; including use of the Örebro.
The wash up…
Psychosocial factors are an important component in a biopsychosocial approach to patient management. Through screening, exploration and triaging of patients based on psychosocial factors, practitioners are more likely to obtain consistently good clinical outcomes!
If you’re interested in a free eLearning module on this and other topical issues click here, subscribe and follow the links.
I’d love to have a dialogue with the Physiopedia audience so feel free to comment below.
Until next time
Jon Ford
References
- Dagenais, S., A. C. Tricco and S. Haldeman (2010). “Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines.” The Spine Journal 10(6): 514-529.
- Ford, J. J. and A. J. Hahne (2013). “Pathoanatomy and classification of low back disorders.” Man Ther 18(2): 165-168.
- Jones, M. and D. Rivett (2004). Introduction to clinical reasoning. Principles of Clinical Reasoning in Manual Therapy. M. Jones and D. Rivett. Oxford, Butterworth-Heinemann.
- Jull, G. and A. Moore (2012). “Hands on, hands off? The swings in musculoskeletal physiotherapy practice.” Manual Therapy 17(3): 199-200.
STOPS back pain as part of Knowledge and Learning Solutions International is declared an educational institution under s.10 of the Copyright Act 1968. This notice is published in accordance with s.10A(4) of The Act.
