Last month, WebPT shared a blog on CMS’s new G-codes in a cleverly titled post, “Ain’t Nothin’ But a G-Code, Baby.” As the name implies, this new mandate is not nearly as daunting as you may think. Here, I’ll discuss how with just a few steps, and some clinical judgment, you can easily implement these new codes within your documentation workflow.
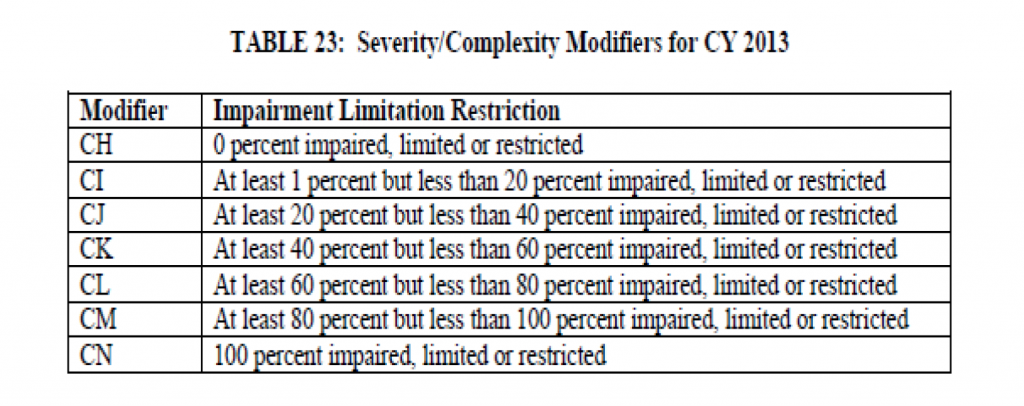
Let’s start with the basics. G-codes are codes you’ll use to describe your patient’s functional limitation—the primary reason he or she is seeking your therapeutic services. You’ll need to assign a current and projected goal status G-code to every Medicare patient during the initial evaluation; at minimum every tenth visit; and at discharge. Every time you apply a G-code, you will also apply a modifier to indicate your patient’s level of impairment. So, how do you determine which modifier to apply? Take the score of the appropriate outcome measurement tool, pair it with a little clinical expertise, and then select the corresponding modifier.
Still fuzzy? Here’s an example:
Mobility: Walking & Moving Around G-Codes
- G8978 Mobility: walking and moving around functional limitation, current status, at therapy episode outset and at reporting intervals.
- G8979 Mobility: walking and moving around functional limitation, projected goal status, at therapy episode outset, at reporting intervals, and at discharge or to end reporting.
- G8980 Mobility: walking and moving around functional limitation, discharge status at discharge from therapy or to end reporting.
Example
Your new patient “Will” has sought your physical therapy services following a total hip replacement. For this example, we can establish Will’s primary functional limitation as Mobility: Walking & Moving Around. Because this is Will’s initial examination, the corresponding G-code is G8978. Now for the modifier. Appropriate to Will’s current condition, you’re going to select the lower extremity functional scale—an outcome measurement test (or one like it) that you should be performing on Will even without this new mandate. Will scores a 5; based on the test scoring rules that means he is at 6.25% of maximal function—or 93.75% impairment—which corresponds to modifier CM. So, Will’s current status on his initial examination would be G8978 CM GP. You’d want to make sure that this code appears on the claim you submit to billing for the initial exam.
Now, let’s tackle his goal. You’ll select G8979, the code under Mobility: Walking & Moving Around that applies to projected goal status, and assign to it the CI modifier because we believe that by the end of treatment Will will improve to at least 1% but less than 20% impairment. You’d want to make sure that G8979 CI GP also appears on the claim you submit to billing for the initial exam.
At the tenth visit, Will’s G-code remains the same (G8978) and you perform the same outcome measurement tool. As a result of your treatment, Will’s score improves to an 18; this means he’s at 22.5% of maximal function—or 77.5% impairment—which corresponds to modifier CL. So, Will’s current status on his tenth visit is G8978 CL GP. Unless there is any change to your goal for Will, his projected goal status code remains the same at G8979 CI GP. You’d want to make sure that G8978 CL GP and G8979 CI GP appear on the billing claim you submit to Medicare for this progress Note visit. You may not bill the re-evaluation code 97002 just for submitting these codes; you may only bill 97002 may if this is truly a re-evaluation—which is a whole different blog post.
On the 20th visit, Will’s progress is outstanding, and he scores a 75 on the lower extremity functional scale; this means he’s at 93.75% of maximal function—or 6.25% impairment—which corresponds to modifier CI. Will has met his goal so you discharge his primary functional limitation with G-code G8980, the code under Mobility: Walking & Moving Around that applies to discharge status (G8980 CI GP). The projected goal status code remains the same at G8979 CI GP. These codes will again appear on the billing claim for this date of service.
Unless you identify a new primary functional limitation at this point, you must discharge Will from therapy. In this case, let’s say that Will is also experiencing wound healing capacity limitation. This doesn’t fall under any of the other functional limitation categories, and this is the first time you are assessing this limitation, so you select G8990, Other PT/OT Primary Functional Limitation, as Will’s new primary functional limitation. Based on your assessment, you decide to perform the South West Regional Wound Care Toolkit and determine he has a 50% wound healing limitation, which corresponds to modifier CK. Thus, Will’s new G-code is G8990 CK GP. This would appear on the billing claim on this 20th visit date of service. You can now continue to see the patient with wound care as your primary limitation. Treatment and documentation of treatment must now reflect this primary limitation. As treatment continues for this patient, you will repeat the steps listed above at the 30th visit and so forth through the discharge of the patient.
Other PT/OT Primary Functional Limitation
- G8990: Other physical or occupational primary functional limitation, current status, at therapy episode outset and at reporting intervals.
- G8991 Other physical or occupational primary functional limitation, projected goal status, at therapy episode outset, at reporting intervals, and at discharge or to end reporting.
- G8992 Other physical or occupational primary functional limitation, discharge status at discharge from therapy or to end reporting.
Now that we’ve knocked that example out of the park. Here are a few additional things to consider:
- You must perform a functional outcome measurement during every assessment (examination, 10th visit minimum/progress note, and discharge) and use the score, along with your own clinical judgment, to select the appropriate modifier.
- There may be instances where your functional outcome measurement tool provides a score that does not directly correlate to the available modifiers. In this case, you must use your judgment and clinical expertise to make a selection. More than anything, though, make sure you are consistent.
- Always restate the projected goal status you implement in your patient’s long term goal. Should this goal change for any reason, document that.
- If your patient’s functional limitation does not fit into one of the predefined categories, you can use the “other” category.
- According to the APTA, if you use tools like FOTO, you can report composite functional scores by using the “other” category (G8990, G8991, and G8992). If the patient achieves their goal and there is a second condition, you should use the G-codes G8993-G8896 for “other subsequent” functional limitation.
- Don’t forget to contact your billing service or billing software vendor to ensure they can properly process the G-codes before they are mandatory in July.
And there you have it: implementing G-codes. I discussed the basics, went through an example, and highlighted some key considerations. Still got questions? Well, I’m ready to dish some answers. Send ‘em to [email protected].
About the Author
Heidi Jannenga, PT, MPT, ATC/L
Heidi was a scholarship athlete at the University of California, Davis. Following a knee injury and subsequent successful rehabilitation, Heidi developed a passion for physical therapy. She started her 16-year physical therapy career after graduating with her Masters from the Institute of Physical Therapy in St. Augustine, Florida.
In 2008, Heidi and her husband Brad launched WebPT, the leading web-based Electronic Medical Record (EMR) and comprehensive practice management service for physical therapists. As the company’s COO, Heidi is responsible for product development/management, billing services, and customer support.
She now resides in Phoenix with Brad and their daughter Ava.