Knee Osteoarthritis
Osteoarthritis causes pain and decreased functional capacity and thus is a common reason for people to seek advice from physiotherapists. While characterized by the irreversible loss of articular cartilage from the condyles of the femur and plateau of the tibia, knee OA is considered a whole joint disease with changes seen in the synovium, ligaments, sub-chondral bone and muscles (Wieland et al. 2005). As the symptoms progress the sufferer is generally forced to reduce their physical activity due to pain and joint restriction resulting in decreased fitness and an increasingly sedentary lifestyle as well as possibly obesity which is associated with numerous co-morbidities e.g. diabetes and stroke. Further, knee OA has wrongly considered by many as a wear-and-tear disease and therefore exercising is considered dangerous and naturally avoid. Unfortunately, activity avoidance results in accelerated progression of the symptoms and loss of functional capacity. However, the current OARSI guidelines list land-based exercise (strength or aerobic training) as a corner stone for the non-surgical management of knee osteoarthritis. Additional interventions include weight management, water-based exercise and self-management as well as education as the core treatments for all individuals (McAlindon et al. 2014). Exercise, irrespective of the type or intensity (Lange, Vanwanseele & Fiatarone Singh 2008), neuromuscular (Ageberg, Link & Roos 2010, Ageberg & Roos 2015) or aerobic (Roddy, Zhang & Doherty 2005), has been shown to be effective at decreasing pain and improving functional capacity in people with knee OA. Prevention is better than cure, so they say. The focus of management of knee OA is now shifting from managing end-stage symptoms i.e. pain and functional deficits, to preventing the progression of the disease including slowing or halting the loss of articular cartilage, i.e. chondroprotective management (Murray, Benke & Mandelbaum 2016, Roos & Arden 2016). Therefore, an optimal exercise intervention should decrease pain, improve function (including lower-limb biomechanics) and preserve the health of the tissues e.g. cartilage. Nevertheless, pain is a known major modulator for activity avoidance in patients with knee OA, often preventing participation in exercise and decreasing physical activity (Holla et al. 2014). Aquatic exercise has long been used and shown to be effective in the management of knee OA (Waller et al 2014) due to it perceived pain reducing effect during and immediately after exercise (Denning, Bressel & Dolny 2010, Roper, Bressel & Tillman 2013).
Aquatic exercise for knee OA
Traditionally, managing knee OA in the water was termed as aquatic therapy, aquatic physiotherapy or hydrotherapy. In my recent systematic review, I used the term therapeutic aquatic exercise (TAE) which I feel is a much more suitable term to describe appropriate prescription of aquatic exercise in the management of knee OA. In this review (Waller et al. 2014) and more recently supported in a recent Cochrane Review (Bartels et al. 2016), we demonstrated that TAE evokes a significant improvement in pain and physical functioning in subjects with lower-limb OA. However, in both systematic reviews, the outcomes had been measured using patient-reported outcomes, i.e. questionnaires, which are notorious at over estimating the size of the treatment effect. When including objective measures of physical function e.g. walking speed, muscle strength and joint ROM, there was either only a very small or no effect evoked by aquatic exercise (Waller et al. 2014). This is concerning especially considering that our most recent systematic, exploring the effects of aquatic exercise on function in healthy older adults, indicated that aquatic exercise evokes significant improvements in different aspect of physical function i.e. muscle strength, walking ability and agility (Waller et al. 2016). The main explanation of the discrepancy was the difference in the exercise interventions and aims of the studies i.e. the OA studies aimed to improve pain and in general used low intensity exercise while the healthy older adult studies primary goal was to improve functional capacity and used interventions of high intensity or designed to impact a specific aspect of functional capacity (Waller et al. 2016).
Transition from traditional to state-of-the-art aquatic exercise for knee OA
Based on recent research aquatic exercise irrespective of type e.g. swimming, deep water running, aquatic calisthenics and intensity evokes an acute decrease in pain and there is a significantly lower levels of pain experienced during aquatic exercise than land-based exercise at equivalent intensities (Denning, Bressel & Dolny 2010, Roper, Bressel & Tillman 2013, Fisken et al. 2014). Therefore, when treating knee OA it seems sensible to focus on focusing on the specific needs of the patients e.g. cardiovascular fitness, muscle power or endurance, flexibility/joint ROM, neuromuscular control of the knee and lower-limbs. While this seems logical, current guidelines and systematic reviews, while differentiating between types of land based exercise modalities e.g. strength, aerobic exercise, have combined all types of aquatic intervention together as one exercise modality. This makes identifying the optimal aquatic exercise intervention difficult. The aquatic exercise program prescribed to each patient with knee OA should be unique to the patient following a full assessment of the patients’ symptoms and goals related to activities and participation as per the ICF. The diversity of the exercises available for this patient group is reflexed in the aquatic exercise module in PhysioTools. Based on clinical experience and current scientific literature I have divided aquatic exercise for people with knee OA into four main exercise groups. The program ideally should be focused on one main outcome (Juhl et al. 2014) and completed at least twice a week (Waller et al. 2016). Short duration aquatic exercise interventions (3-6 months) generally only have short term benefits in this population and the therapist must therefore build in to the management plan long-term adaptations to the patient’s physical activity habits in order to achieve long term sustained benefit.
Flexibility and joint ROM
Static stretching in warm water may be easier than land; the buoyancy of water also allows the use of flotation devices to be use to aid the stretch and allow the patient to “relax” into the stretch (Figure 1). In research by our research group it appears that muscle spindle activation decreases during passive immersion (active immersion is yet to be fully investigated) (Pöyhönen & Avela 2002, Cronin et al. 2016), this in combination with decreased pain, may allow more effective passive soft-tissue stretching. Additionally, there is growing evidence that active full range of motion exercise repeated many times may evoke similar improvements in joint range of motion as passive methods in chronic diseases while facilitating an impact on the contractile elements of the muscle. Further active movements impact the extra-cellular matrix through thixotropy, improved cell activity in the fascia and increased tissue temperature, thus aiding improving in flexibility and mobility of the soft-tissues. Through clinical observations, in this patient group, passive stretching should be reserved for the cool down, specific muscle groups not easily activated through full ROM and when pain prevents active movements.
Aquatic resistance training
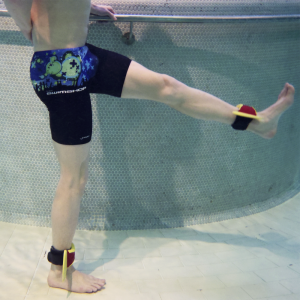
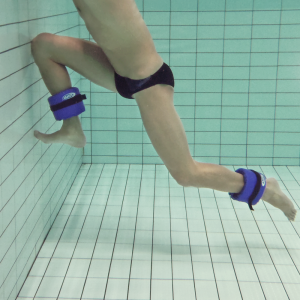
The recommendation for prescription of resistance training is based on the application of a percentage of the individuals 1 repetition maximum (1RM). Low intensity strength training involves 10-15 repetitions at 40% of 1RM, moderate is 6-10 repetitions at 40-60% of 1 RM and high is 6-8 repetitions >60% of 1RM(AGS Clinical Practice Committee 2001, Nelson et al. 2007). Prescribing resistance training in water, compared to land, is much more difficult as there are currently no methods to externally control the work done by the muscles. One method for controlling resistance during aquatic resistance training is the use of equipment that increases the surface area of the limb (Pöyhönen et al. 2000). The addition of a large resistance boot (Figure 2) to the lower limb significantly increases drag forces during under water movement, even though there is a reduction in angular velocity (Pöyhönen et al. 2001). In healthy women, drag forces produced during knee flexion and extension exercises in water with large resistance boots were 145N ± 30 compared to barefoot conditions of 45N ± 13 during knee extension; during knee flexion, the corresponding values were 145N ± 30 and 55N ± 13 (Pöyhönen et al. 2001). This highlights the importance of utilising equipment to provide additional resistance to progress and optimise the effect evoked from aquatic resistance training. Significant benefits have been observed with a progressive aquatic resistance training programme for physical functioning in healthy women (Pöyhönen et al. 2002b), women with mild knee OA (Munukka et al. 2016) and following knee arthroplasty (Valtonen et al. 2010). Each of these studies utilised program consisting of 5-6 lower limb exercises lower-limb aquatic resistance exercise focusing on the knee extensors and flexors as well the hip flexors, extensors, abductors and adductors. Each exercise was completed for 30-60 seconds with the encouragement to complete each repetition “as hard and fast as possible”. Typically, each leg was consecutively exercised without rest followed by 30-45 seconds of rest with 2-4 sets per exercise, with 1 minute rest between each exercise. This protocol can be, and has been, modified according to the desired response i.e. muscle power, power-endurance or muscle endurance, patients’ current level of fitness and possible other co-morbidities. Overall each program lasted approximately 30-40 minutes of high intensity exercises which was preceded with a 10-15 minute warm and afterwards with a 10 minutes of light aerobic exercises and lower muscle stretching. The participants completed this program three times a week for 12-16 weeks. The improvements in neuromuscular function suggest that this exercise modality could be used to treat the pain and decreased functional capacity e.g. muscle strength and walking ability in people with knee OA. Moreover, no injury has been reported from these three studies (Pöyhönen et al. 2002a, Valtonen et al. 2010, Munukka et al. 2016) as result of this intervention. In fact very few serious injuries or harm has been documented as a result of aquatic exercise in people with lower OA (Waller et al. 2014) and in healthy older adults (Waller et al. 2016) at any intensity.
Cardiovascular fitness

When aerobic exercise is prescribed for an OA patient, its intensity may be assessed by using a rating of perceived exertion (RPE) or a percentage of V02max or heart rate maximum which has been previously measured on land. The type of aquatic exercise utilised to improved cardiovascular fitness is not as important as the intensity the exercises are performed at. The training modality can be according to patient preference, e.g. deep water running (Figure 3), calisthenics, high repetition aquatic resistance exercises and swimming. Aquatic exercise for improvements in cardiovascular fitness should be performed 3-5 times a week for 30-60 minutes and follow recommended guidelines: moderate intensity is described as RPE 5-6/10 (40-60% of V02 max/HR max) and 7-8/10 (60-80% of V02 max/HR max) for vigorous (AGS Clinical Practice Committee 2001, Nelson et al. 2007). Heart rate and V02max vary extensively between different aquatic exercise modalities and individuals (Denning et al. 2012). Optimally, training intensity should be set using pre-intervention measures values of either absolute or estimated cardiovascular fitness (VO2); however these are not often feasible on land for this population due to pain or lack of compliance. Recently, protocols for measuring aerobic capacity during deep-water running and shallow water walking have been developed and validated for patient populations. The results of these tests provide the basis for accurately monitoring the intensity of an individualised aquatic training programme (Cuesta-Vargas & Heywood 2011, Benelli et al. 2014). Setting an individualised target training intensity during aquatic exercise appears to be very important for overall improvements; when fitness testing is not available or possible, the use of rating of perceived exertion or target heart estimated with the Karvonen equation (Maximum heart rate = 220 – age) are still valid methods for prescription of aerobic aquatic exercise.
Neuromuscular and balance exercise

Neuromuscular training has been shown to decrease the frequency of knee injuries (Gagnier, Morgenstern & Chess 2013) as well as improve function and decrease pain in people at risk of knee OA (Roos & Dahlberg 2005) and suffering from knee OA (Ageberg & Roos 2015). Neuromuscular training is recommended in individuals with knee OA but the appearance of pain can affect the proprioceptive feedback during exercise (Knoop et al. 2011). The aquatic exercise programme devised by Hinman et al. (2007), integrates many common aspects of land-based neuromuscular training, while using the body weight supporting effect of buoyancy to assist the movement (Hinman, Heywood & Day 2007). This program used double and single leg squats, steps up (Figure 4), lunges and calf raises. This type of program may be useful initially, with a gradual decrease in water depth to increase weight-bearing as a way to increase exercise tolerance before transferring to land. However, these exercise really only utilise buoyancy whereas
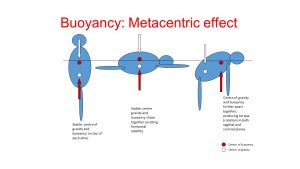
popular swimming teaching and aquatic therapy methods use the interaction between the forces of gravity and buoyancy, i.e. the meta-centric effect (Figure 5). Simply put; when a body is immersed in water it is exposed to both the up-thrust from buoyancy and “down thrust” from gravity. When these two forces are in-line with each other the body (person) is stable but when the forces are not inline they create torque which results in rotation of the body unless muscle activation prevents it. A simple example is seen in figure 6, where a traditional neuromuscular exercise, e.g. a lunge, can be progressed at the mid-point of the movement by lifting one hand slightly out of the water thus creating torque. This rotation torque is described by the plane in which the rotation occurs, i.e. sagittal rotation in the case of this example; this is the reasoning for the terminology in many of the trunk activation/control exercise in the PhysioTools module. While under researched, these neuromuscular type exercises typically make up at least 40% of an aquatic exercise programs I have prescribe to patient with not only knee OA but after ACL and knee and hip surgery.



Summary
The prescription of therapeutic aquatic exercise to people with knee OA should focus on trying to improve the patient’s own individual symptoms and functional impairments which are both affecting the patients’ quality of life as well as present a risk for progression of the disease. While focusing on pain and self-reported improvements in function, aquatic exercise should primarily be prescribed with the aim to improve specific aspects of function capacity and the training intensities should represent this.
Read more about the PhysioTools module Aquatic Therapy by Ben Waller.
Bibliography
Ageberg, E., Link, A. & Roos, E. M. 2010. Feasibility of neuromuscular training in patients with severe hip or knee OA: the individualized goal-based NEMEX-TJR training program. BMC musculoskeletal disorders 11, 126-2474-11-126.
Ageberg, E. & Roos, E. M. 2015. Neuromuscular exercise as treatment of degenerative knee disease. Exercise and sport sciences reviews 43 (1), 14-22.
AGS Clinical Practice Committee 2001. Exercise prescription for older adults with osteoarthritis pain: Consensus practice recommendations. Journal of the American Geriatrics Society 49 (6), 808-823.
Bartels, E. M., Juhl, C. B., Christensen, R., Hagen, K. B., Danneskiold-Samsoe, B., Dagfinrud, H. & Lund, H. 2016. Aquatic exercise for the treatment of knee and hip osteoarthritis. The Cochrane database of systematic reviews 3, CD005523.
Benelli, P., Colasanti, F., Ditroilo, M., Cuesta-Vargas, A., Gatta, G., Giacomini, F. & Lucertini, F. 2014. Physiological and biomechanical responses to walking underwater on a non-motorised treadmill: effects of different exercise intensities and depths in middle-aged healthy women. Journal of sports sciences 32 (3), 268-277.
Cronin, N. J., Valtonen, A. M., Waller, B., Poyhonen, T. & Avela, J. 2016. Effects of short term water immersion on peripheral reflex excitability in hemiplegic and healthy individuals: A preliminary study. Journal of Musculoskeletal & Neuronal Interactions 16 (1), 58-62.
Cuesta-Vargas, A. I. & Heywood, S. 2011. Aerobic fitness testing in chronic nonspecific low back pain: a comparison of deep-water running with cycle ergometry. American Journal of Physical Medicine & Rehabilitation 90 (12), 1030-1035.
Denning, W. M., Bressel, E., Dolny, D., Bressel, M. & Seeley, M. K. 2012. A Review of Biophysical Differences Between Aquatic and Land-Based Exercise. International Journal of Aquatic Research & Education 6 (1), 46-67.
Denning, W. M., Bressel, E. & Dolny, D. G. 2010. Underwater treadmill exercise as a potential treatment for adults with osteoarthritis. International Journal of Aquatic Research and Education 4, 70-80.
Fisken, A., Waters, D. L., Hing, W. A., Steele, M. & Keogh, J. W. 2014. Perception and Responses to Different Forms of Aqua-Based Exercise Among Older Adults With Osteoarthritis. International Journal of Aquatic Research & Education 8, 32-52.
Gagnier, J. J., Morgenstern, H. & Chess, L. 2013. Interventions designed to prevent anterior cruciate ligament injuries in adolescents and adults: a systematic review and meta-analysis. The American Journal of Sports Medicine 41 (8), 1952-1962.
Hinman, R. S., Heywood, S. E. & Day, A. R. 2007. Aquatic physical therapy for hip and knee osteoarthritis: results of a single-blind randomized controlled trial. Physical Therapy 87 (1), 32-43.
Holla, J. F., Sanchez-Ramirez, D. C., van der Leeden, M., Ket, J. C., Roorda, L. D., Lems, W. F., Steultjens, M. P. & Dekker, J. 2014. The avoidance model in knee and hip osteoarthritis: a systematic review of the evidence. Journal of Behavioral Medicine 37 (6), 1226-1241.
Juhl, C., Christensen, R., Roos, E. M., Zhang, W. & Lund, H. 2014. Impact of exercise type and dose on pain and disability in knee osteoarthritis: a systematic review and meta-regression analysis of randomized controlled trials. Arthritis & rheumatology (Hoboken, N.J.) 66 (3), 622-636.
Knoop, J., Steultjens, M. P., van der Leeden, M., van der Esch, M., Thorstensson, C. A., Roorda, L. D., Lems, W. F. & Dekker, J. 2011. Proprioception in knee osteoarthritis: a narrative review. Osteoarthritis and cartilage 19 (4), 381-388.
Lange, A. K., Vanwanseele, B. & Fiatarone Singh, M. A. 2008. Strength training for treatment of osteoarthritis of the knee: a systematic review. Arthritis and Rheumatism 59 (10), 1488-1494.
McAlindon, T., Bannuru, R., Sullivan, M., Arden, N., Berenbaum, F., Bierma-Zeinstra, S., Hawker, G., Henrotin, Y., Hunter, D. & Kawaguchi, H. 2014. OARSI guidelines for the non-surgical management of knee osteoarthritis. Osteoarthritis and Cartilage 22 (3), 363-388.
Munukka, M., Waller, B., Rantalainen, T., Hakkinen, A., Nieminen, M. T., Lammentausta, E., Kujala, U. M., Paloneva, J., Sipila, S., Peuna, A., Kautiainen, H., Selanne, H., Kiviranta, I. & Heinonen, A. 2016. Efficacy of progressive aquatic resistance training for tibiofemoral cartilage in postmenopausal women with mild knee osteoarthritis: a randomised controlled trial. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society .
Murray, I. R., Benke, M. T. & Mandelbaum, B. R. 2016. Management of knee articular cartilage injuries in athletes: chondroprotection, chondrofacilitation, and resurfacing. Knee surgery, sports traumatology, arthroscopy 24 (5), 1617-1626.
Nelson, M. E., Rejeski, W. J., Blair, S. N., Duncan, P. W., Judge, J. O., King, A. C., Macera, C. A. & Castaneda-Sceppa, C. 2007. Physical activity and public health in older adults: recommendation from the American College of Sports Medicine and the American Heart Association. Circulation 116 (9), 1094.
Pöyhönen, T. & Avela, J. 2002. Effect of head-out water immersion on neuromuscular function of the plantarflexor muscles. Aviation, Space, and Environmental Medicine 73 (12), 1215-1218.
Pöyhönen, T., Keskinen, K. L., Hautala, A. & Mälkiä, E. 2000. Determination of hydrodynamic drag forces and drag coefficients on human leg/foot model during knee exercise. Clinical Biomechanics 15 (4), 256-260.
Pöyhönen, T., Keskinen, K. L., Kyrölainen, H., Hautala, A., Savolainen, J. & Mälkiä, E. 2001. Neuromuscular function during therapeutic knee exercise under water and on dry land. Archives of Physical Medicine & Rehabilitation 82 (10), 1446-1452.
Pöyhönen, T., Sipilä, S., Keskinen, K., Hautala, A., Savolainen, J. & Mälkiä, E. 2002a. Effects of aquatic resistance training on neuromuscular performance in healthy women. Medicine and science in sports and exercise 34, 2103-2109.
Pöyhönen, T., Sipilä, S., Keskinen, K. L., Hautala, A., Savolainen, J. & Mälkiä, E. 2002b. Effects of aquatic resistance training on neuromuscular performance in healthy women. Medicine & Science in Sports & Exercise 34 (12), 2103-2109.
Roddy, E., Zhang, W. & Doherty, M. 2005. Aerobic walking or strengthening exercise for osteoarthritis of the knee? A systematic review. Annals of the Rheumatic Diseases 64 (4), 544-548.
Roos, E. M. & Arden, N. K. 2016. Strategies for the prevention of knee osteoarthritis. Nature reviews.Rheumatology 12 (2), 92-101.
Roos, E. M. P. T. & Dahlberg, L. 2005. Positive Effects of Moderate Exercise on Glycosaminoglycan Content in Knee Cartilage: A Four-Month, Randomized, Controlled Trial in Patients at Risk of Osteoarthritis. Arthritis & Rheumatism 52 (11), 3507-3514.
Roper, J. A., Bressel, E. & Tillman, M. D. 2013. Acute aquatic treadmill exercise improves gait and pain in people with knee osteoarthritis. Archives of Physical Medicine and Rehabilitation 94 (3), 419-425.
Valtonen, A., Pöyhönen, T., Sipilä, S. & Heinonen, A. 2010. Effects of aquatic resistance training on mobility limitation and lower-limb impairments after knee replacement. Archives of Physical Medicine and Rehabilitation 91 (6), 833-839.
Waller, B., Ogonowska-Słodownik, A., Vitor, M., Rodionova, K., Lambeck, J., Heinonen, A. & Daly, D. 2016. The effect of aquatic exercise on physical functioning in the older adult: a systematic review with meta-analysis. Age and Ageing , doi: 10.1093/ageing/afw102.
Waller, B., Ogonowska-Slodownik, A., Vitor, M., Lambeck, J., Daly, D., Kujala, U. M. & Heinonen, A. 2014. Effect of therapeutic aquatic exercise on symptoms and function associated with lower limb osteoarthritis: systematic review with meta-analysis. Physical Therapy 94 (10), 1383-1395.
Wieland, H. A., Michaelis, M., Kirschbaum, B. J. & Rudolphi, K. A. 2005. Osteoarthritis—an untreatable disease? Nature reviews Drug discovery 4 (4), 331-344.
