The Struggle
For years, I despised treating the insertional Achilles tendon pain patient. I tried everything I was told by different gurus. One well-established ankle and foot orthopedist swore by heel lifts and prolonged stretching off a step: 3 minutes, 3x/day and you would get better. The next told me to place patients in a walking boot to unload the insertion. Another podiatrist requested I ultrasound and ice massage them. My PT Mentors told me to exercise them.
At this point, my head was spinning and I begged not to see these patients anymore. Finally, I began to see the light. For some reason, this condition is poorly understood, causing it to not be treated properly. To effectively treat it, we really need to understand why it is happening.
Overcome Those Tricky Tendinopathies
Understanding the MOI
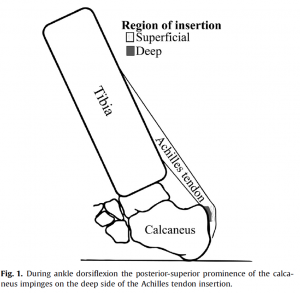
It is not that the Achilles or calf is too tight as many had suggested to me. It’s certainly not that we only need a modality-based treatment plan. A walking boot may help in the short-term, but it does not fix the cause. What actually occurs is that when the ankle moves into excessive, loaded dorsiflexion, the deep layers of the Achilles tendon are compressed against the calcaneal tubercle. Instead of having a condition that is caused by a stretch like so many of us often believe, it is truly a compressive or shearing that is driving the issue as shown in Chimenti’s1 diagram.
Once we understand that, it seems that stretching would only compress the tissue even greater. Instead, we need to find ways to help patients avoid this excessive dorsiflexion when in a loaded position. Running hills, excessive stair walking, and any other activity where the ankle may be unable to control itself will be problematic. This even includes a commonly prescribed PT exercise: Calf raises through the full range of motion off a step. We are contributing to the problem!
Instead, a more proper treatment plan would temporarily remove the stressor, look to control against future stress, and finally re-introduce normal movement.
The Plan
Here’s an example outline:
Step 1: Initial Treatment Plan
- Heel lift to reduce dorsiflexion and resultant compression on the deep Achilles tendon
- Isometrics in a slightly plantarflexed position
- Modalities as chosen to help reduce symptoms
Step 2:
- Maintain pain-free ADLs through use of heel lift
- Begin calf raises from a slightly elevated surface to improve calf control
- Place a small text book under the heels to avoid DF or even loaded neutral
Step 3:
- Phase out of heel lift without pain during ADLs
- Re-introduce calf raises through an increasing ROM
Step 4:
- Re-introduce all functional activities including plyometrics and running hills
This is a combination of an established protocol described by Jonsson et al2, which showed a 67% patient satisfaction rate using calf raises and Chimenti et al’s1 description of the benefits of a heel lift. Additionally, we can use Sibernagel et al’s3 thoughts on progressing programs and find a very well rounded plan for a patient that is going to be successful more often than not.
Often, patients can continue running throughout the plan, but should avoid hills and plyometrics due to the increased load in dorsiflexion. If the patient has higher level symptoms or the post-run pain does not dissipate, then they may need to take a short break from running.
Additionally, Steps 1-4 should not be looked at for every patient. If the patient does not require Step 1 and can jump right to Step 2 due to low irritability, this is great! If the patient is not a runner/athlete, you may never move through Step 4. The best outcomes occur when you combine guidelines such as these and make the appropriate adjustments for the patient in front of you.
Looking for more? Join us for a Certified Gait Analyst Course.
Just want a taste? Check out Doug Adams’s e-book on posture and running.
References
- Chimenti RL, Flemister AS, Ketz J, et al. Utrasound strain mapping of Achilles tendon compressive strain patterns during dorsiflexion. J of Biomech. 2016;49:39-44.
- Jonsson P, Alfredson H, Sunding K, et al. New regiment for eccentric calf-muscle training in patients with chronic insertional Achilles tendinopathy: Results of a pilot study. Br J Sports Med. 2008;42:746-749.
- Silbernagel KG, Crossley KM. A proposed return-to-sport program for patients with midportion Achilles tendinopathy: Rational and implementation. J Orthop Sports Phys Ther. 2015;45(11):876-886.