What do you think about when you see the word “Frail”. Do you think of an older person, or somebody who is sick, maybe you think of people who are physically unable and weak, or all/none of the above? Do you think frailty has any relation to living with HIV? Just take a moment… consider what you are thinking.
Currently academic discussions have emerged in recent years, discussing if people living with HIV are experiencing frailty. This is especially relevant as we know that people living with HIV on treatment, can live normal life expectancies, and people are growing older with HIV. In addition, I previously discussed the disability and multi-morbidity that can be experienced by people living with HIV, and interestingly in the general population a causal relationship has been described between comorbidities, disability and frailty; whereby comorbidity is a risk factor, and disability an outcome of frailty. The evidence however, may suggest that people living with HIV experience frailty at earlier ages than HIV-negative counterparts. But to understand and explore this further, we need to first understand frailty.
Unfortunately I need to admit to you there is no “gold standard” definition of frailty. In fact there are several definitions; so I am going to discuss the two most accepted conceptualised models (in no particular order) of frailty to get us started.
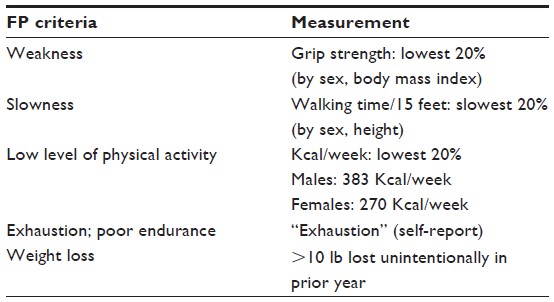
The Frailty “Phenotypic” model by Fried; where frailty is a distinct process defined by deficits in multiple physiologic systems. Meaning a loss of physical reserve. It includes 5 components; shrinking or unintentional weight loss; muscle weakness; poor endurance and energy; slowness in walking speed; and low levels of physical activity. The presence of 3 or more of the 5 components is considered frail, and 1 or 2 components as pre-frail. There are also resources available online to facilitate a standardised approach to assessing the Fried frailty model in clinical settings.
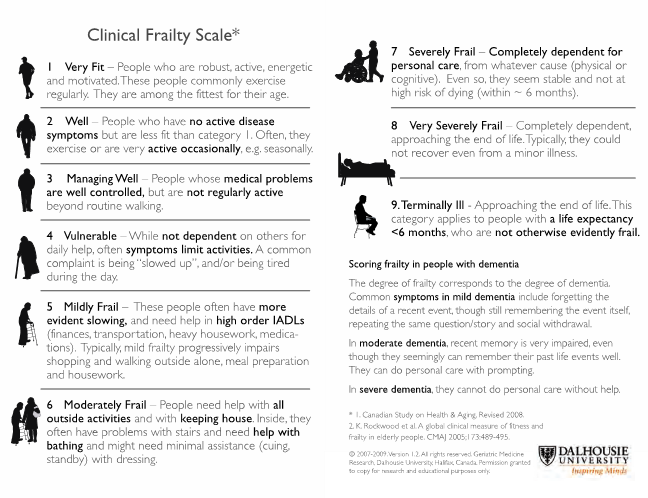
The Frailty “Cumulative Deficits” model by Rockwood; where frailty is the vulnerability associated with accumulation of multiple health deficits. Meaning the more health conditions you have, the more likely you are to be frail. The associated “Frailty Index” is a count of 70 clinical deficits, and is able to quantitatively summarise vulnerability to frailty however is not practical for use in clinical settings due it’s size. Therefore the Clinical Frailty Scale was developed for clinical settings, and has been shown to be an effective measure of frailty and provides similar predictive information as the frailty index.
Fried’s “Phenotypic” model of frailty is the most commonly used frailty measurement among people living with HIV, and studies using this model demonstrate higher rates of frailty occurring at younger ages in both North America (with studies also focusing on women and injecting drugs users) and Europe.
Interestingly the Frailty Index based on the “Cumulative deficits” model has only been used in one study. However the Veterans Ageing Cohort Study (VACS) Index developed to assess physiologic frailty, including routine clinical HIV and organ system biomarkers, has been accepted as an effective frailty measure, predicting hospitalisation, intensive care admission and fragility fractures. The presence of frailty and HIV can predict mortality, therefore measuring frailty is important to identify the most vulnerable and help target resources.
HIV appears to be independently associated with frailty, and frailty is associated with increased falls risk, broken bones, unemployment and social isolation. Yet no known HIV standards or guidelines internationally advocate frailty measurement into routine care. Could this be a silent epidemic that we are not preparing for or responding too?
This is where I Segway rehabilitation, but specifically Physiotherapy, into the discussion. Physiotherapists are experts at routinely measuring a number of the parameters used to define frailty eg: physical function, strength, endurance / exhaustion, walking speed and engagement in regular physical activity. Physiotherapists also routinely address these areas, for example providing and supporting individualised exercises to improve cardiorespiratory fitness and aerobic endurance, muscle strength and power, improving balance and reducing falls risk. Exercise is the medicine to reverse or mitigate frailty, preserve quality of life, and restore independent functioning in older adults at risk of frailty, and is recommended for frail older adults. Physiotherapists are described as having the “golden-bullet” to address frailty, because…
Physiotherapy Works for frailty
Physiotherapists provide exercise-based interventions for people with disability and movement challenges, therefore are perfectly placed to address frailty among people living with HIV who cannot engage in exercise independently. Physiotherapists already have the skills to address these issues related to frailty because they are already doing this for the general population with services such as cardiac rehabilitation, pulmonary rehabilitation, pain management services and falls prevention services. In the general population of England, Physiotherapy interventions could prevent 187,000 serious falls per year and save the NHS £275million annually; for every £1 spent of Physiotherapy, there is a cost gain of £1.50.
But Physiotherapists are not routine members of the multi-disciplinary team for people living with HIV internationally; even when rehabilitation is recommended for older adults living with HIV. In the absence of the inclusion of allied health professionals such as Physiotherapists into the existing HIV service delivery models, we need to identify the networks or services, that people living with HIV can access or be referred too. However the caveat here is that this could only work if we measure frailty (and more widely disability) to identify those most at risk, to allow all people living with HIV to access rehabilitation for the improvement of health and well-being.
Frailty is not associated simply with increasing age. We need to redefine ageing among people living with HIV into phenotypes eg: disability, frailty, accelerated ageing and successful ageing; that should be discussed in relation to comorbid and cognitive ageing. If we successfully introduce measuring frailty into clinical practice, we can start to address the gaps. If we identify the size of the issue, we can plan the workforce required to prevent, reverse and manage frailty with the inclusion of Physiotherapists into HIV care services.
So what do you now think about when you see the word “Frail”?