Evidence informs us that we should use psychological interventions when managing low back pain but which treatment is best?
Fear avoidance, anxiety, depression, social stress and catastrophic thinking are highly prevalent in people living with LBP and can increase pain and risk of disability. This is why most clinical guidance considers psychological treatments as essential when treating chronic low back pain.
Think About Managing LBP Differently
The difficulty is there are numerous psychological treatment options available and the lack of information means it’s difficult for clinicians to know which treatment option is best and in what circumstance.
A new systematic review published in the BMJ set out to determine the comparative effectiveness and safety of psychological interventions for low back pain.
Methods
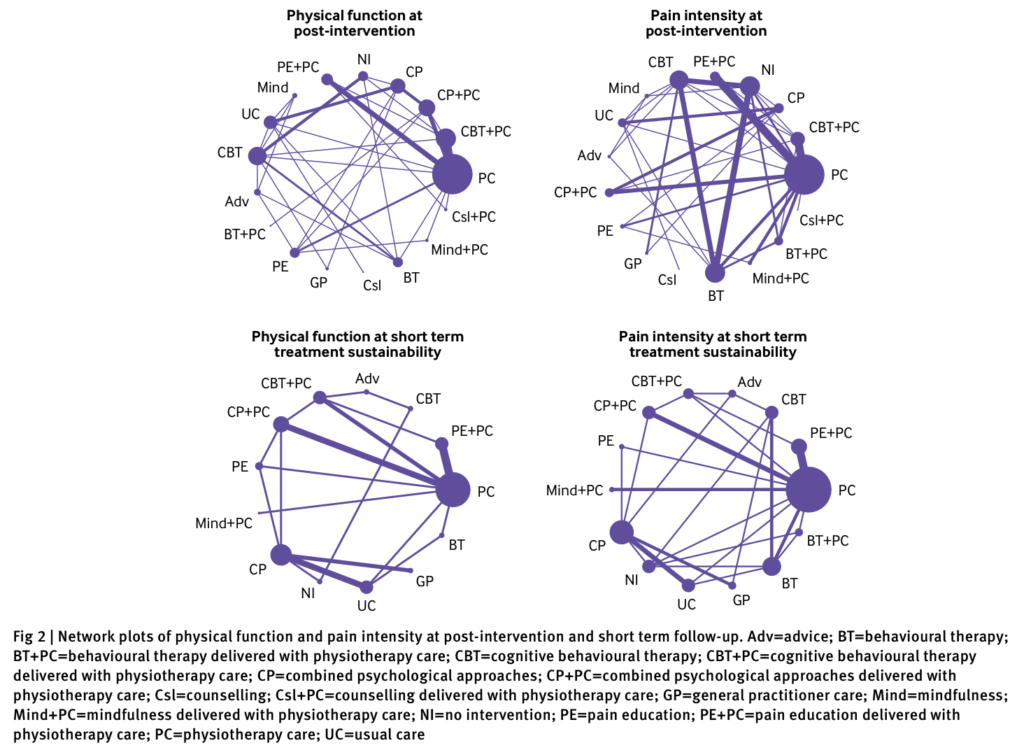
This systematic review with network analysis adhered to PRISMA guidance and the protocol was pre-registered on PROSPERO. Eight databases were used for the search which took place on 31st January 2021, with the search strategy combining an exhaustive list of concepts, language, and keywords for randomised controlled trial, LBP, and psychological interventions. The search strategy is available in full for each database.
To be included within the review studies had to meet the following criteria:
- Be a randomised controlled trial (parallel, cluster or cross over) which were published in peer reviewed journals
- Include participants who were 18 or older and had experienced chronic, non-specific low back pain according to the NICE definition
- Compared psychological interventions with any comparison intervention
For the purposes of this systematic review a psychological intervention can include any of the following:cognitive behavioural therapeutic strategies, mindfulness based stress reduction, acceptance and commitment therapy, cognitive functional therapy, health coaching, biofeedback (delivered with a therapeutic intent to promote muscle relaxation), pain education, and counselling directly using principles of psychological theory. More details about treatment definitions are available in the supplementary information.
The primary outcome measure of interest was physical function and pain intensity of the lower back. Secondary outcomes were fear avoidance, health related quality of life, intervention compliance and safety. Outcomes were measured up to 12 months after the first treatment. The Cochrane Risk of Bias Tool 2.0 was used to assess for bias.
Results
In total 97 studies involving 13, 126 people were included within the systematic review. Most studies were published between 2011 and 2021 and were conducted in Europe. Physiotherapy intervention was the most common comparison intervention. The general characteristics of the participants was pretty equal across the studies however reporting of socioeconomic information was inconsistent with only 1/3 of studies consistently reporting this information. This is a limitation considering the impact of socio-economic background on interventions for LBP.
On average the included studies were judged to have a moderate risk of bias with a few having high risk. The most common source of bias pertains to measurement of outcome and selection of reporting result. Sensitivity analysis show that despite these concerns the results were not greatly affected.
Psychological Interventions for Physical Function
61 studies (n= 9, 397) assessed physical function with CBT + physio and pain education + physio being the two most effective treatments at short and medium term (6-12 months). CBT + physio saw the biggest improvement in physical function (SMD 1.01, 95% CI 0.58 to 1.44) with results equivalent to 19.6 point increase on a scale of 0-100. Pain education + physio had an equivalent increase to 12.0 points on a 0-100 scale. After 12 months it appears that neither treatment is more effective than physio alone.
Psychological Interventions for Pain Intensity
66 studies (n= 9462) assessed pain intensity and when the results are pooled together there are three interventions which appear to have large and clinically significant effects on reducing pain intensity when compared to physio alone. Behavioural therapy + physio was most effective with an increase equivalent to 27.3 points on a 0 – 100 scale followed by CBT + physio and pain education + physio. No other combination of treatments were more effective than physiotherapy alone.
Summary and Clinical Importance
Chronic pain conditions require multimodal biopsychosocial treatment approaches. This systematic review demonstrates that in conjunction with physio interventions CBT, pain education and behavioural therapy are effective treatment choices for improving pain intensity and physical function in people living with chronic LBP.