Approximately 75% of all limb fractures are reported as simple, stable fractures. For these fractures a virtual fracture clinic can offer a high quality more efficient model of care than traditional fracture clinics. But which fractures best suit a virtual approach?
It is estimated that approximately 10% of emergency department attendanced require an orthopaedic review. As the number of emergency admissions is continually rising this is putting increased demand on an already overloaded orthopaedic services. This combined with a reduced number face to face clinic appointments and clinic space becaue of COVID-19 means different models of care are required to meet ensure patient outcomes are unaffected.
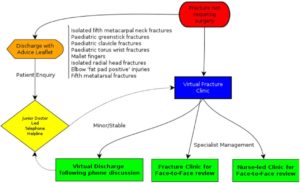 Virtual clinics have been used by many orthopaedic teams alongside traditional fracture clinics since the early 2010’s. This evoluton in service provision was triggered by the creation of the Glasgow Fracture Pathway. There is a large number of studies published on the different experiences of institutions of using VFCs. One example is shown in the diagram on the right from West Middlesex Hospital in London.
Virtual clinics have been used by many orthopaedic teams alongside traditional fracture clinics since the early 2010’s. This evoluton in service provision was triggered by the creation of the Glasgow Fracture Pathway. There is a large number of studies published on the different experiences of institutions of using VFCs. One example is shown in the diagram on the right from West Middlesex Hospital in London.
Their VFC pathway is specifically designed for paediatric upper limb fractures and adult wrist and hand fractures. Other VFCs target shoulder dislocation and stable fractures, others on the lower limb, different VFCs evolve based on local demand and capabilities. Generally though, VFCs are used as an alternative in the management of common undisplaced simple fractures.
Good Virtual Communication is Essential for Successful VFCs
A new systematic review published in Injury this week set out to clearly define the cohort of injuries which most benefit from a virtual approach. This is the first systematic review to do so and has come at an important time as we adjust to new ways of working.
Method
PIRMSA guidelines have been adhered to however the review was not PROSPERO registered. A brief and broad search strategy was used and has been published in full and the databased searched were MEDLINE, EMBASE and Cochrane Library. As a minimum three are expected to be used and according to Cochrane these three are generally considered adequate.
Methodological quality of the included evidence was assessed using The Cochrane Collaboration Risk of Bias Tool. Data extraction inclued patient demographics, clinical outcomes, patient reported outcomes and cost analysis of clinic visit. Data was analysed using SPSS.
In total 15 studies were included for analysis, this was from an initial serach result of 13,555 studies. The 15 studies totally 11,921 patients with 52% being male with an average age of 41. It is worth noting that over half of this patient population came from a single study.
Frustratingly several of the studies only reported fractures as ‘simple’ or ‘stable’ making overall analysis difficult as unclassified fractures do not help answer the hypothesis.
Results and Clinical Implications
The results of the systematic are below.
- The rate of discharge to GP/Physiotherapy was 65.7%
- 81% of patients were satisfied with VFCs
- The average cost saving per patient using VFC pathway was £53 compared to TFC
- Most evidence exists for 5th metatarsal and radial head and neck fractures
- Limited definitive evidence for all other types of fractures being supported in VFC’s exists but that’s not to say it isn’t possible or safe
In summary there is reasonable evidence to support VFCs for 5th metatarsal fractures with moderate evidence for radial head and neck fractures. Due to under reporting of fracture type and location is it hard to draw further conclusion.
