Psoriatic arthritis is a complex condition but can be managed with physiotherapy. Below we will talk you through which treatments you need to include.
Psoriatic arthritis is chronic progressive inflammatory joint disease that can be associated with a number of extra-articular manifestation such as psoriasis. The clinical hallmark is the presence of peripheral and axial arthritis, dactylitis, enthesitis and psoriasis.
Deep Dive into Spondyloarthropathy
In recent years new drugs have revolutionised the management of the condition however some patients either are unable to tolerate or are unfortunately unresponsive to treatment. For these patients physiotherapy plays a crucial role in managing their symptoms.
Even if patients respond and tolerate pharmacological treatment exercise should still form a central part of treatment regimines. But what exercise is most effective in this population and what treatments should we use if patients a unresponsive to drug management?
A new narrative review has set out to explore the evidence on the role of physical therapy, exercise and rehabilitation in the management PsA patients in each disease domain.
Methods
Pubmed and the Cochrane Library were searched for relevant articles using the following search terms: ‘‘psoriatic arthritis,’’ ‘‘psoriasis,’’ ‘‘psoriatic disease,’’ ‘‘synovitis,’’ ‘‘axial involvement,’’ ‘‘dactylitis,’’ ‘‘enthesitis,’’ ‘‘rehabilitation,’’ ‘‘exercise,’’ ‘‘physical therapy’’ and ‘‘comorbidities,’’. The search was date limited between 1st January 2000 to 30th October 2020. Human clinical studies, clinical trials, reviews and meta-analyses were included.
Results & Clinical Take Home
As the name of the condition suggests psoriasis is a key extra-articular manifestation of the condition. Psoriasis is an inflammatory condition with itchy, red, scaley plaques and not everyone with psoriasis has psoriatic arthritis however it is a key symptom to be aware of. Generally speaking for patients with psoriatic arthritis their psoriasis will be mild. The condition can have a severe impact on quality of life.
Obesity, alcohol consumption, smoking, poor sleep hygeine and sedentary lifestyles have all been associated with worsening psoriasis therefore modification of these behaviours will have a positive effect on the condition. The same can be said for stress which is known to be a significant trigger for exacerbations of the skin conditon.
This is why relaxation, basic exercise, mindfulness and behavioural and lifestyle modification therapies have been shown to be effective at reducing Psoriasis Area and Severity Index (PASI) scores. Clinically this is why a multi-disciplinary team approach is important for this patient group. Get Psychologist, Dietitian and Occupational Therapy involvement early in your management plan for you patients with psoriatic arthritis.
Peripheral Involvement- Dactylitis and Axial Involvement
The majority of patients living with psoriatic arthritis will have an erosive and osteo-proliferative arthritis. This is where disease-modifying anti-rheumatic drugs (DMARDs) are crucial as they alter the course of the disease process and ultimately delay the destruction of the articular surfaces.
With regards to DMARDs exercise and physiotherapy treatment should focus on different aspects of a patients health in order to maximise the effectiveness of pharmacological therapy and reduce the side effect burden as well as help increase the overall potential ultimate potential duration of DMARD effectiveness.
Additionally basic exercise and physiotherapy treatment modalities should not be overlooked. Cryotherapy can be effective in helping to reduce joint pain, swelling and tenderness improving adcitivities of daily living. Splints and orthoses are possibly useful in reducing the risk of articular deformity however evidence is limited. Hydrotherapy may be a useful treatment option for patients with high levels of pain and low confidence with independent exercise.
Exercise is key to life-long management of the condition and is recommended by the EULAR guidelines for people with inflammatory arthritis inclusing psoriatic arthritis. This however is general advice and mostly adheres to the 150 minutes of exercise a week with a mixture of exercise types. This reflects the lack of research and evidence for specific exercise protocols and strategies in this patient population. There are emerging studies investigating HIIT training in this population however outcomes have not shown alteration to the disease process rather only improvements in fatigue.
Treatment of dactylitis in people living is psoiratic arthritis follows similar recommendations to rheumatoid arthritis. Maintenance of function and range of movement of the small joints of the hand is the central treatment objective. This is complemented by helping patients find alternative, less painful ways of carrying out daily activites. Thermal modalities also help achieve these objectives.
Axial disease in psoriatic arthritis shows some similarities with axial spondyloarthropathy and therefore the role of exercise in the management of spinal symptoms has the same relevance and importance.
Enthesitis – Difficult to Manage
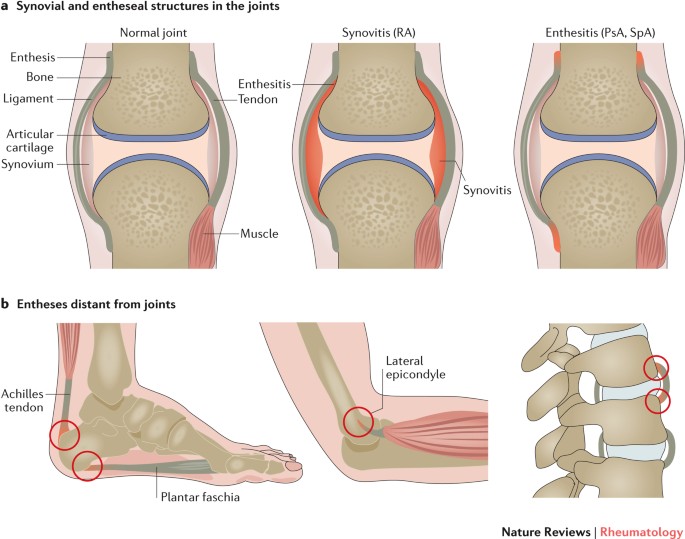
Enthesitis presents in around 1/3 to 1/2 of people living with psoriatic arthritis. According to this narrative review there is little evidence for the physiotherapeutic treatment of this symptom. That being said it is still a symptoms we need to be aware of as clinicians as it can be a significant barrier to participating in exercise due to the location and pain caused by movement.
Enthesitis typically presents as pain, stiffness and tenderness of insertions without much swelling. However, swelling may also be a feature in larger insertions of the lower limbs. Enthesitis is diagnosed clinically with pain elicited on local pressure of entheseal points, or through use of imaging; magnetic resonance imaging or ultrasonography.
Clinically, enthesitis may be difficult to recognise without the presence of swelling. The enthesis is a relatively avascular structure therefore inflammatory markers such as ESR or CRP may not be elevated in entheseal-related disorders. Additionally many insertions are either inaccessible to the examiner and present with poorly localised pain.
Basic, regular stretching is a good place to start particularly before participating in exercise. Evidence for laser therapy and shockwave therapy is severly lacking and it isn’t recommended at this stage even considering the theoretical beenfit of stimulating self-repair activity of living tissue.
Co-Morbidities – Mitigate the Increased Risk
Psoriatic arthritis is associated with several co-morbidities due to the presence of the chronic underlying inflammation of the condition itself. It has been suggested that patients have a 43% increased risk of developing cardiovascular disease. This includes a 68% increased risk of heart attack, 22% increased risk of stroke and 31% increased risk of heart failure. It is important to consider that this a relative risk not absolute risk.
Because of the increased risk of cardiovascular disease exercise and dietary modification is crucial in mitgating this increased risk. This is why the EULAR Psoriatic arthritis treatment guideline recommends exercise not only to reduce the buden of disease but also to treat cardiometabolic comorbidities.
Overall this review suggests that current evidence demonstrates the potential benefts of exerise and physiotherapy in patients with psoriatic arthropathy. However, the volume and quality of evidence is lacking which means exact protocols of treatment is uncertain.
This post was originally published March, 2021 and written by Scott Buxton. The page has now been updated for freshness, accuracy and comprehensiveness.