With more physio’s working in primary care than ever before we need to ask the question, is physio a cost effective alternative to doctors?
One of the most common musculoskeletal conditions seen in primary care is knee osteoarthritis. It is also a condition physiotherapists and physicians are comfortable with seeing when undiagnosed making it an ideal condition to compare health and economic outcomes.
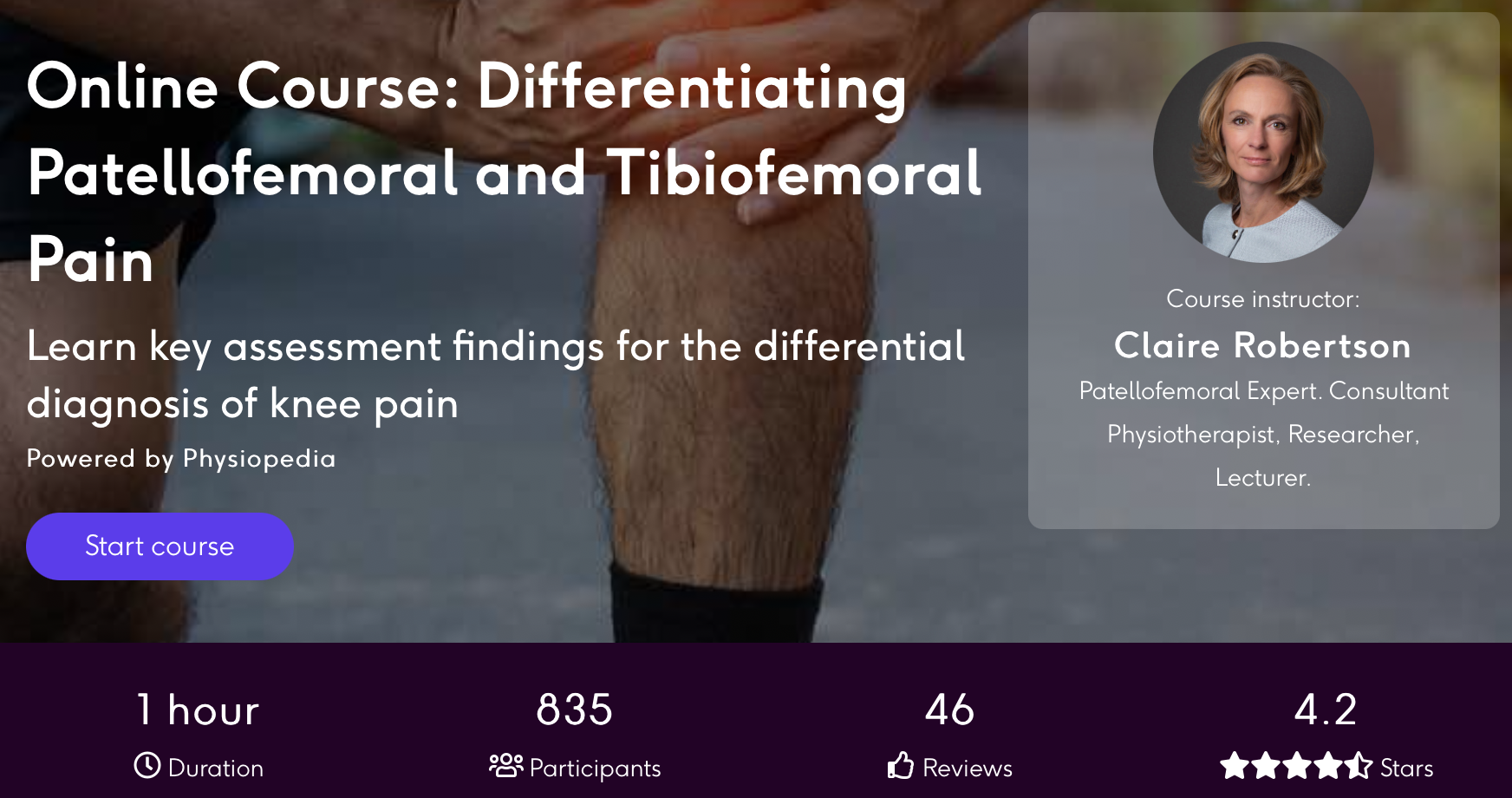
Improve Your Knee Pain Differentials
Several studies exist which demonstrate the diagnostic agreement between physiotherapists and doctors but it’s less clear which is more cost effective particularly in primary care. Furthermore with the increase in the number of physiotherapists working in primary care in a first contact role, it’s important to understand if seeing a physio first rather than a doctor is beneficial for the patients.
This is exactly what a new study published in BMC Musculoskeletal Disorders has set out to clarify by comparing health and economic outcomes between a physio first and physician first.
Methods
The protocol of this cost-effectiveness analysis alongside an assessor-blinded RCT has been published in full. The trial took place in Sweden between 2013-2017 and therefore, the cost analysis factored in Swedish societal perspectives limiting some aspect of the findings to elsewhere. Particularly countries with weaker welfare and healthcare support for the local population.
There was a total of 69 patients included within the review with 35 in the physio first group and 34 in the physician first group. This was an adequate sample size according to power analysis. Both physio and physician used national guidance in their diagnostic and treatment approach with the only significant different between the physician having access to radiography.
The treatments available to the physio were either individual or group based exercise and advice based the Better Management of OA (BOA) programme. The physician treatment could include information, medication and referrals to radiography, physiotherapy or another healthcare professional.
Demographic data, BMI, pain intensity using VAS and physical function using the 30s chair stand test were all used as physical outcome measures. HrQOL and EQ-5D-3L were the generic health outcome measures used with follow up over 3, 6 and 12 months with results also available as QUALY.
The cost effectiveness evaluation was calculated in retrospect after the final follow up at 12 months. A lot of data was collected to calculate the total healthcare cost including referrals, administrative time, telephone calls, prescriptions, productivity losses and clinician time. The calculations and financial assumptions required to complete the analysis are available in the study.
Results
There was a total drop out rate of 36% across the two groups with slight more dropping out of the physician first group (11 compared to 14). Regardless of whether a patient saw a physician or physio first, the majority saw a physio during their treatment. There were 26 patients who only had physio and 14 who only had physician consultations.
Seven patients in the physiotherapist group consulted a physician as well, and 14 patients in the physician group sought a physio for further treatment. On average, patients in the physiotherapist group consulted a physio four times individually plus two group visits and had 0.3 physician visits. Patients who had a physician as primary assessor had on average 1.5 physician visits and four individual physio visits plus 1.5 group visits.
Patients who saw a physio were less likely to be referred for radiography and we also less likely to be referred to an orthopaedic surgeon. Patients were more likely to be prescribed medication if saw by the physician first.
Comparing the costs for the two groups using a societal perspective shows that the physio first group was cheaper than the physician first group (633 ± 620€/patient vs 996 ± 1276€/patient) and these results remain consistent when using average costs from a healthcare perspective (515 ± 541€/ patient vs 748 ± 885€/ patient). On average it looks to be about 300€ cheaper to see a physio first.
In terms of QALYs both physio first and physician first groups gained 0.74 and 0.75 respectively at 1 year after first visit. This slightly higher score in the physician first group means that patients gain slightly less QALYs but at a lower cost when assessed by a physio first. However when confidence intervals were calculated the overlap leads to no real-world differences.
It’s important to consider the limitations of this study. The study was based in Sweden with a small and limited sample size which greatly limits replicability and applicability elsewhere. Furthermore the economic landscape has greatly changed since 2017 meaning the cost assumptions will have changed if the study would be performed now. Direct access to physiotherapy in primary care is still rapidly evolving and perhaps if this study were to be repeated now the outcomes would be different.