It’s been one year of article of the week and there are many lessons we can learn from the publications we’ve covered. As we approach the end of the academic year and the transition from student to new graduate let’s cover the essential lessons from article of the week!
Follow The Example of These Clinical Trials & Physiotherapy Research Has a Promising Future
Physiotherapy research has come along way in the past decade however there are still many publications published which come under criticism for being under powered, lacking methodological rigour and lacking generalisability. So what makes a great physiotherapy clinical trial?
2020 signalled the 20th aniversary of PEDro, the Physiotherapy Evidence Database and to celebrate PEDro physiotherapists were asked to nomicate RCTs published between 2015-2019 that answered important clinical questions.
The submissions were judged by an expert panel and they nominated a top 5 based on innovation, clinical impact and robust methodology. Looking at these top five articles we can draw out themes which are hallmarks of high quality physiotherapy research which we can all use to direct future research. The top five were:
- LIPPSMAck POP– Lung Infection Prevention Post Surgery – Major Abdominal with Pre-Operative Physiotherapy
- SARAH – Exercises to Improve Function of The Rheumatoid Hand
- AVERT– Efficacy and Safety of Very Early Mobilisation Within 24hrs of Stroke Onset
- HIHO – Effect of Inpatient Rehabilitation vs A Monitored Home-Based Program on Mobility in Patients with Total Knee Arthroplasty
- UK FASHIoN – Hip Arthroscopy Versus Best Conservative Care for The Treatment of Femoroacetabular Impingement Syndrome
Arguably the most important commonality between all 5 studies is that they aimed to answer important clinical questions which challenge conventional thinking and result in immediate implications for clinical practice.
Clinical Prediction Rules for Musculoskeletal Practice Shouldn’t Be Trusted
Clinical prediction rules (CPRs) are tools that intend to guide clinicians in their everyday clinical decision making. They provide an evidence-based tool to assist in patient management when diagnosing or when predicting a response to a particular intervention. They tend to be prescriptive in nature and are increasing in popularity but is this a good thing?
Some believe there has been too much focus on the creation of new CPRs rather than validating and updating the existing ones so a team set out to evaluate the current situation through a systematic review which evaluated how the most common CPRs were created and if they actually did what they set out to achieve accurately.
The findings of the systematic review show that many CPRs are created without validation making is difficult to support their use in clinical practice. Even those CPRs which did have validation studies often suffered methodological flaws. If you are using a CPR in clinical practice assess the validity of the tool prior to its use.
Don’t Overlook Online Learning – It’s Just as Good as Hands On!
Physiotherapist pride themselves on their clinical accumen and practical skills, and rightly so. Practical skills are woven into the fabric of our education but does this preference towards practical education limit our opportunities to explore more effective and accessible forms of education?
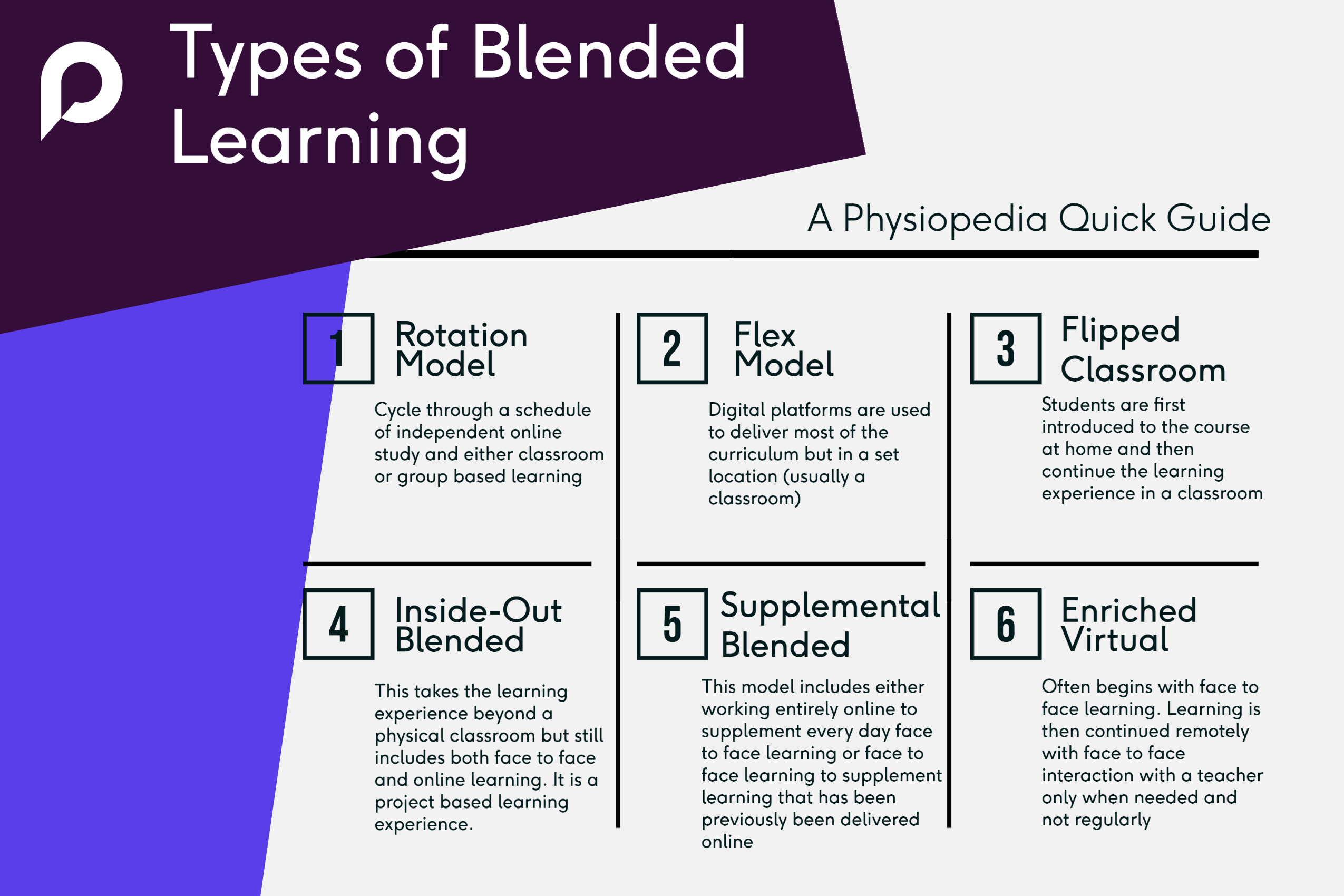
Until the pandemic digital and blended learning approaches have not been fully embraced by our profession and have been criticised for not being grounded from a theoretical learning perspective. This is contrary to evidence which for a long time has demonstrated the effectiveness of using digital learning for healthcare education however there is still debate on the topic.
A systematic review was published in early 2021 which aimed to clarify the effectivenss of digital and blended learning designs in physiotherapy and put this debate to bed once and for all. The systematic review, which was of high standard demonstrated that:
- Blended learning is likely more effective than traditional classroom teaching in physiotherapy education for both knowledge and practical skill acquisition
- Students preferred flipped classroom, interactive website / apps and self-produced videos rather than traditional classroom experiences which also translated into better learning effects
- MCQ’s offer a useful and effective learning tool
The main take away from this systematic review is that blended learning showed at least equal if not statistically better learning outcomes compared to traditional methods. We should no longer bias our approaches to hands on education only.
Courses Improve Clinical Practice More Than Journal Articles
Late in 2020 an interesting survey was published in the BJSM which explored which resources used to alter their clinical practice. To some the results might be somewhat of a surprise, to others it might be a confirmation of long held opinion, but clinicians don’t use journals to alter their clinical practice. Instead courses and peer-to-peer learning lead to direct clinical changes.
They survey used data from over 2,000 clinicians and by far the most common way clinicians learned was through peer-to-peer discussion (52%). A surprising outcome was that clinicians prefer using journal articles was a more popular way of changing clincial practice than a podcast, SoMe post or YouTube video. Perhaps this is to do with the trustworthiness of the sources, quality of content or just the fact that as a profession we are still adjusting to online / virtual CPD.
It would be interesting to repeat this survey now we have been through the multiple ways of the pandemic. It’s likely the way out profession learns and changes clinical practice has changed forever.
Try a Discussion with a Difference
Understanding How To Understand a Systematic Review is Important
Systematic reviews are one of the most reliable ways of using journal articles to alter your clinical practice. Often they are the only way we can address questions that couldn’t be answered by individual studies alone and they are a vital resource for clinicians, researchers, patients and policy makers alike. However, they only achieve this role when they are transparent, accurate and complete including the why’s and what’s of the review itself.
The Preferred Reporting Items for Systematic review and Meta-Analyses (PRIMSA) statement is a guideline designed to ensure that systematic reviews are accurate, complete and transparent. Understanding it is essential to evaluating a systematic review, as like all research bias and methodological error affects applicability to clinical practice.
In 2020 the PRISMA guideline was updated and it is a must read for new graduates, especially as there is growing criticism of not having enough systematic review research methodology exploration in undergraduate education.