We are beginning to understand the long term effects COVID-19 has on lung function. This new systematic review helps quantify the effects and guide evaluation of long term change in lung function.
As our understanding of COVID-19 improves the list of ways the virus affects the lungs grows longer. Although the virus affects several body systems we know the lungs sustain the most damage. Approximately 8% of total cases present with a rapid progressive respiratory failure similar to ARDS and 6% of patients in critical are require ventilatory assistance.
A number of pathological events are thought to affect the lungs of patients with COVID. These include diffuse alveolar epithelium destruction, damage to mucous membranes, capillary damage with haemorrhage, pulmonary consolidation and alveolar septal fibrous proliferation. It is this fibrous proliferation and endothelial damage which is the biggest concern when considering the long term damage and resipartory symtoms found in long COVID.
MDT Involvement Reduced Risk of Long COVID
There are a number of different ways of measuring lung function. The most common are pulmonary function tests (i.e spirometry), x-ray and CT scans. These scans and investigations help determine the concequences of acute or chronic effects of COVID-19 objectively.
The first reports of changes to lung function related to coronavirus indicate that patients have a restrictive defect and small airways dysfunction that can be persistent and not related to disease severity. This is similar to what is known about SARS and MERS infection too, with patients experiencing a reduction in lung function lasting from months to years. The scientific community is yet to definitively know what the pattern or prevalence of long term impairment of lung function from covid-19 infection is, however a number of small scale studies have begun to try to develop our understanding.
A new systematic review has been conducted to pool these studies together to add confidence in our understanding. Specifically to determine the prevalence of restrictive, obstructive and altered diffusion patterns in patients post-COVID-19 infection and to describe the different evaluations of respiratory function to use with these patients.
The results of this systematic review is important as it will give us a clearly understanding of what we need to do clinically to detect changes in lung function for the diagnosis and follow up of patients post-covid-19 infection. This will ensure the risk of long term impairment is mitigated as much as possible.
Methodology
One of the most important parts of a systematic review is the search strategy as without a robust search strategy you can’t be sure you’ve included all the relevant data in your pooled analysis. This is why it is best practice for authors to include the search strategy in full to enable fair and transparent critique and analysis of readers. This article is an excellent of a search strategy being published in full with all boolean operators and quotes for specific key word searching. It is also refreshing to see no language restrictions being imposed on the search results either.
To keep the excellence up the review adhered to PRISMA and the protocol was registered with PROSPERO. The reviewing process was also of high quality with three different experienced systematic reviewers being available to extract data, decide which articles should be included and the third was specifically used if one and two disagreed with each other. Methodological quality of the studies was assessed using the NHLBI tool.
Check Out The Ultimate Guide to COVID-19 for Physiotherapists
Part of the challenge when performing systematic reviews is allowing for publication bias. One way of combating publication bias is seeking unpublished data from studies. One way of achieving this is by looking for relevant trials which were published on pre-publication / trial registration sites and seeing if they were ever published / finished and including the data from these trials within the SR if of good enough quality. This is what the authors of the paper did and this should be commended.
In total 7 studies were included within the review – 6 Chinese studies and 1 French study incorportating 380 post-infection COVID-19 patients.
Results & Clinical Importance
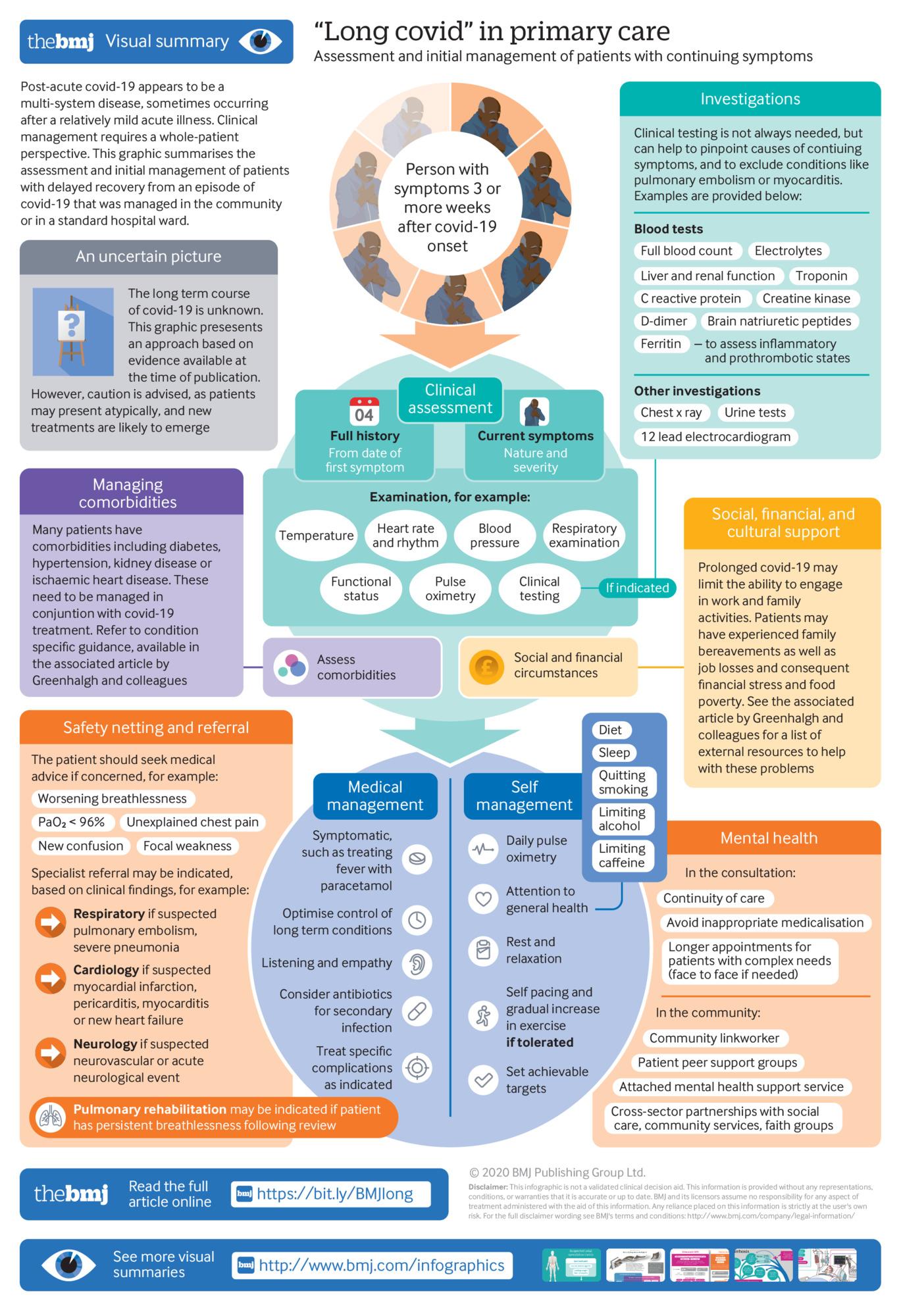
The results of the systematic review show that post-covid-19 patients show varying degrees and severity of altered lung function with diffusion capacity being the most common impairment (~40% of patients). Lung function tests are an important tool in evaluating the long term damage of the virus however caution needs to be applied to interpreting results in those with co-morbidities and those who smoke. We still aren’t sure of which test is best to use however spirometry is a good places to start along with a repeat x-ray 3 weeks after infection if severe enough to be admitted.
The British Thoracic Society recommends the evaluation of pulmonary function tests at 3 months post-discharge from hospital especially for those suspected to have interstitial disease. Current evidence suggests that many tests are taking place only 1 month after onset of infection or 1 month posts discharge. The concequences of hasty evaluation may lead to diagnostic errors.
Although our understanding of the long term effects of covid infection are limited our knowledge is moving quickly. Yes, we may be missing the specifics but we know that if a patient has MDT involvement in their recovery the chances of getting long covid is reduce.