In a nutshell invasive techniques, such as acupuncture, electroacupuncture and dry needling, are likely to help reduce pain severity and improve function in people living with fibromyalgia syndrome. Overall the evidence is of weak quality and therefore this should only remain as an adjunct treatment to exercise.
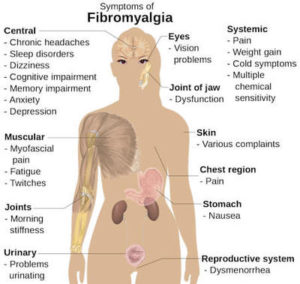 Fibromyalgia is a central sensitivity syndrome defined by a chronic widespread painful state of at least 3 months duration. The symptoms can be diverse which makes the diagnosis of the condition challenging. Muscle rigidity, diffuse paraesthesia, sleep disturbance, depression, migraine, fatigue and mental disturbance (known as fibro fog) have all be proven to be a part of the patient experience.
Fibromyalgia is a central sensitivity syndrome defined by a chronic widespread painful state of at least 3 months duration. The symptoms can be diverse which makes the diagnosis of the condition challenging. Muscle rigidity, diffuse paraesthesia, sleep disturbance, depression, migraine, fatigue and mental disturbance (known as fibro fog) have all be proven to be a part of the patient experience.
The syndrome affects approximately 2% of the global population with women 7 times more likely to suffer from the conditon then men. Interestingly 85% of cases can be found in those between the 4th and 6th decades of life.
In a nutshell our overall understanding of Fibromyalgia syndrome is poor. Currently the exact mechanics of the syndrome are unknown. The existence of localised areas of painful ‘points’ that perpetuate pain impulses is considered an important factor as this conditions the hyperactivity and hyperexcitability of the central nervous system. This drives the central sensitisation process. As well as suffering muscular pain and tenderness the psychological symptoms suffered are a significant part of the condition and are a continuous source of stress which also contributes to increasing levels of pain.
Because the condition is complex and poorly understood fibromyalgia can remain undiagnosed for a long time. Some medical professionals don’t feel that the condition is ‘real’ therefore invalidating the patient’s experience and prevent or even block access to necessary treatments. The stigma around the condition is a serious issue and often drives the conditions intensity. Unfortunately the way pain is taught during training programmes feeds this cycle of stigma and misunderstanding therefore a change to pain education is sorely needed.
It’s Time to Rethink Pain Education
Exercise is the Best Medicine
Exercise and education forms the core management strategies of fibromyalgia. According to Cochrane there is gold level evidence that supervised aerobic exercise training has beneficial effects on physical performance and symptoms of the syndrome. Additionally strength training may also have benefits on some FM symptoms therefore a combined approach of supervised aerobic and strength training is the best strategy.
From a pharmacological point of view traditional common analgesics are ineffective in FMS (including paracetamol and ibuprofen). Medicines that are sometimes used to treat epilepsy or depression can be effective in some people with fibromyalgia. Amitriptyline is a potential useful alternative medicine but it is only thought to be effective in 1 in 4 more than a placebo and a third of these patients suffer adverse effects from the drug. This sums up the difficulty with treating FMS, we don’t really know what works because we don’t understand enough about the condition.
This is one of the reasons supportive and symptom control is the best approach for patients. Anecdotally the use of invasive techniques such as dry needling, acupuncture and electroacupuncture are reported to be effective at reducing pain and improving function in patients. The proposed analgesic mechanism of these invasive treatments are both interesting and complex. At spinal cord level A-beta, A-delta, C-fibres and GABA activation has been shown to occur as well as activation of the endogenous opioid system providing a pain relieving effect.
Other studies have shown that invasive techniques have an effect on psychological wellbeing and mental health thereby reducing severity of pain. But what does the evidence tell us?
Actupuncture Possibly Reduces Pain in People with FMS Although the Evidence Quality is Poor
A new systematic review has been published in the journal Pain Medicine which aims to shed light on the effectiveness of acupuncture and dry needling at reducing pain and improving function in people living with fibromyalgia syndrome. Overall 16 studies were included within the review, 8 for the qualitative analysis and 8 for the quantitative analysis.
The outcome measures used to assess pain intensity were the visual analogue scale Wong-Baker Face Pain Rating Scale with quality of life assessed using the MOSSF-36 or the FIQ.
The research followed systematic review best practice by being registered with PROSPERO and adhering to PRISMA guidelines throughout. The flow chart was published within the article as to is the search strategy. Risk of bias was assessed using CONSORT and the Cochrane RoB tool, both of which are reliable tools to use for this type of research question.
The research followed systematic review best practice by being registered with PROSPERO and adhering to PRISMA guidelines throughout. The flow chart was published within the article as to is the search strategy. Risk of bias was assessed using CONSORT and the Cochrane RoB tool, both of which are reliable tools to use for this type of research question.
The results of this systematic review indicate that there is low quality evidence to suggest that invasive techniques produce a significant reduction in pain intensity and significant improvement in physical function. The effects of invasive techniques are greater in the short term and therefore this treatment choice should be used as an adjunct to long term management strategies such as exercise and cognitive strategies.
Fibromyalgia is one of the most stigmatised conditions around. It is our professions duty to be the leaders in the way we think about pain and help improve the function of patients living with long term complex pain. Why not take a look at this short online course created by Kristine Lew and start to change the way you think about pain.