Sarcopenia should be thought of as a disease; acute or chronic muscle failure. Identification and management should be a priority and a core aim of every physiotherapists when treating see older people.
As we age our muscles undergo progressive changes, primarily involving loss of muscle mass and strength. The age-related loss of muscle function is known as Sarcopenia, derived from the Greek words for flesh (sarcos) and loss (penia) and its definition includes loss of muscle strength and power, as well as reduced function. It occurs with increasing age, and is a major component in the development of frailty.
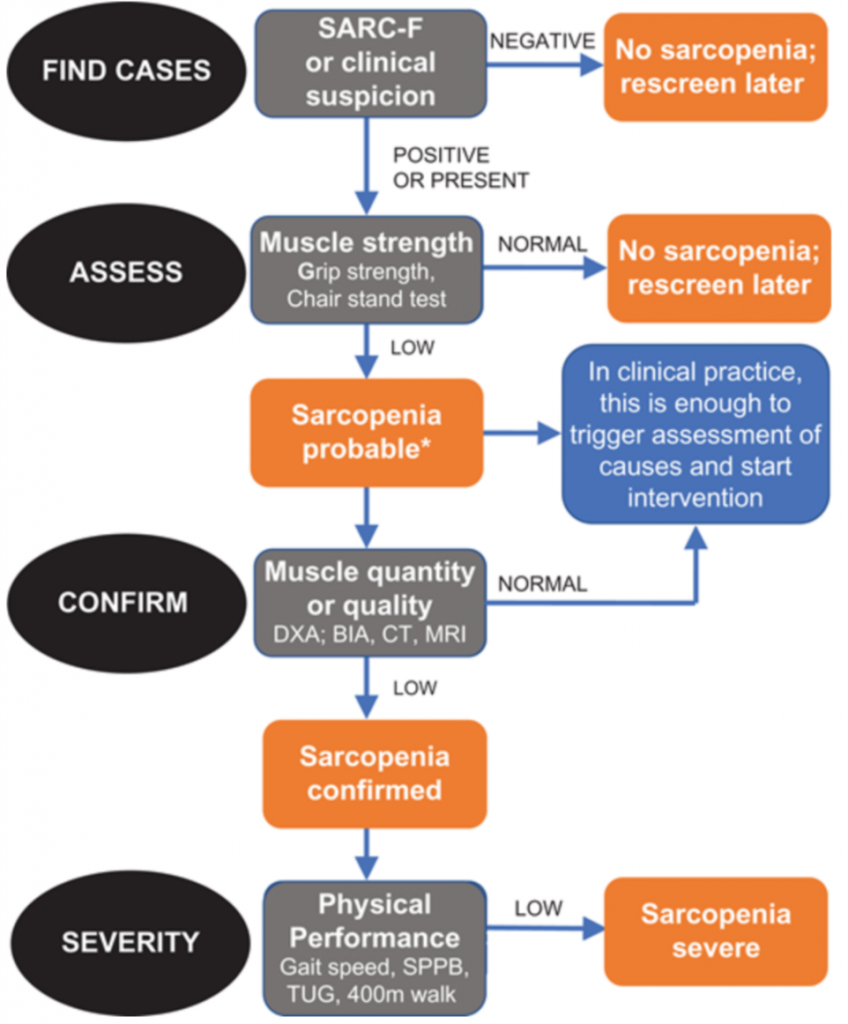
The SARC-F Questionnaire is what EWGSOP 2 recommends for characterisation of sarcopenia. This is a 5-item self-reported questionnaire that has low-moderate sensitivity and very high specificity. It is inexpensive and convenient and will ensure that clinicians identify severe cases of sarcopenia. Therefore it is a great tool to start to introduce the concept of muscle failure into clinical practice.
There are a number of investigations that can reliably quantify the severity of muscle loss in older adults but they are expensive and unavailable to 99% of practicing clinicians. They are interesting nonetheless and are likely to become more commonplace in the future.
Take Lumbar 3rd Vertebrae CT scans as an example. L3-CT correlates significantly with whole body muscle mass as well as accurately predicting prognosis. CT is also useful for investigating mid-thigh muscle mass which is potentially more accurate than L3-CT.
A cheaper and just as accurate alternative to CT is diagnostic ultrasound (USS) and is highly reliable. USS will also inform the user of muscle thinckness, cross-sectional area, fascicle length, pennation angle and echogenicity, all of which surely makes all physios jump at joy. The European Geriatric Medical Society produces a consensus protocol for the use of US in sarcopenia so in all liklihood this will be used in the near future, at least in research, to diagnose sarcopenia.
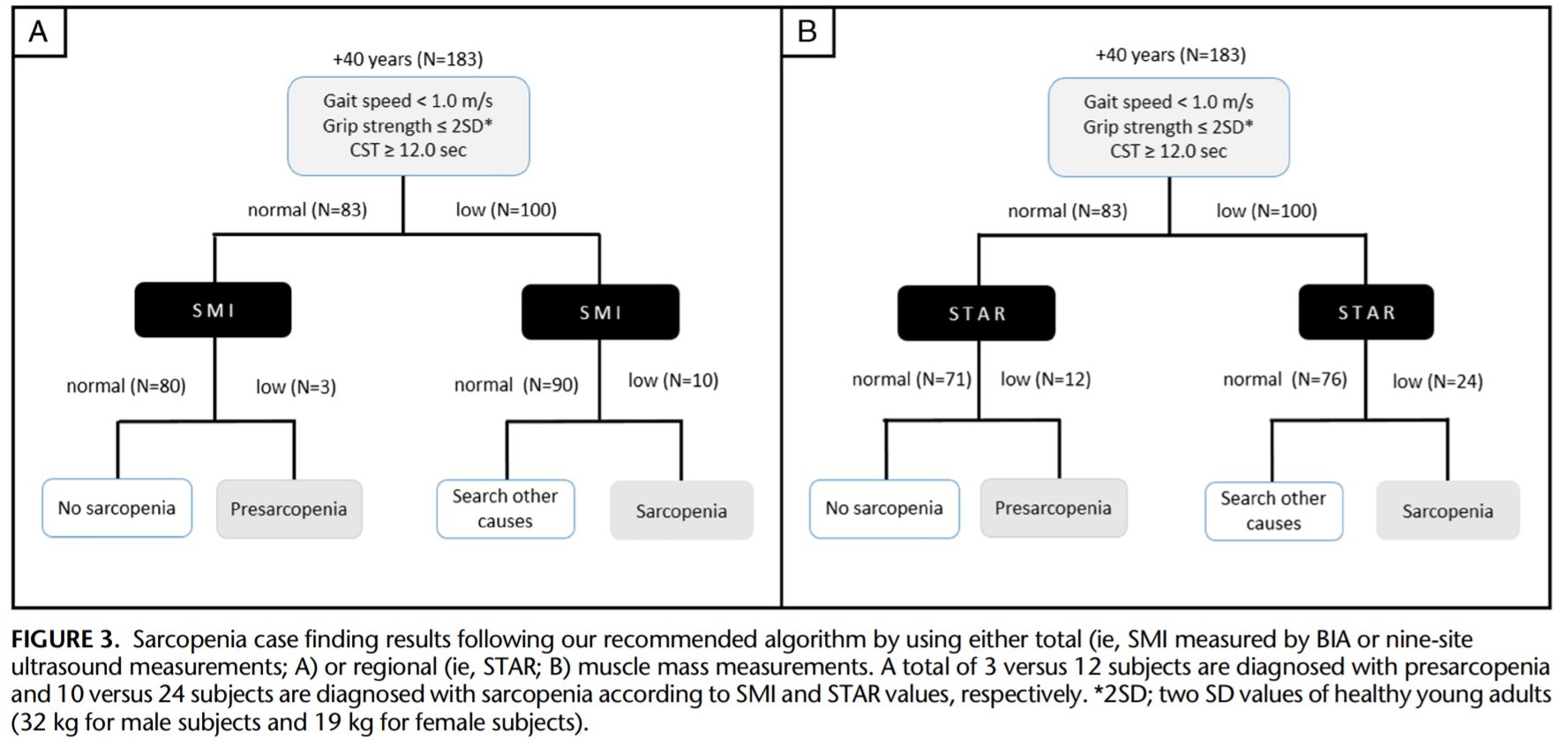
A new cross sectional study involving 326 adults has been published investigating the applicability of USS in diagnosis in a clinical setting. Specifically that regional muscle mass measurement of the quadriceps, using the STAR measurement, rather than total body measurement can reliably be used in the diagnosis of sarcopenia. Interestingly this could also aid early detection however more studies are required to confirm this hypothesis.
STAR= Anterior thig muscle thickness (mm) / BMI (kg/m2)
Clinical Implication
The anterior thigh is often the first muscle mass to be affected by the sarcopenic process and therefore the most likely candidate for consistent and possible early diagnosis. This study looked at the scores using USS and the STAR measurement and a score of 1.0 (female) and 1.4 (male) seem to be useful in diagnosis.