One of the biggest challenges facing any business—rehab therapy private practices included—is effective pricing. Price your product or service too high, and you’ll have a tough time selling enough to stay in the black. Price it too low, and you may end up selling yourself short—literally. And for rehab therapy practitioners who accept third-party payments from insurance plans, payer fee schedules add another layer of complexity to the already-complicated issue of pricing. So, how do you harness your inner Bob Barker and make sure the price is right?
1. Assume that you won’t receive the full amount billed.
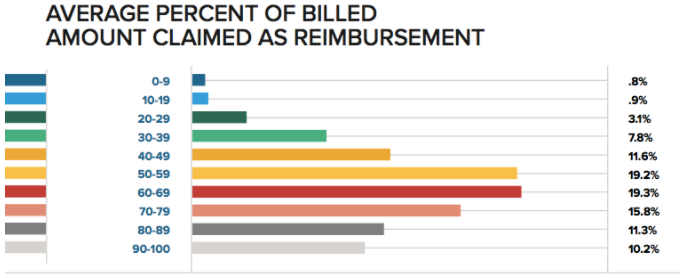
In WebPT’s recent industry-wide survey of more than 5,000 PT, OT, and SLP professionals, we found that four out of five respondents typically received less than 80% of the amount billed per claim, with about 40% of respondents receiving between 50% and 70% of the amount billed.
Those might not sound like great numbers, but they are actually pretty common. In fact, payers rarely reimburse the full amount billed. They usually cover a percentage, and the amount they cover may be below the clinic’s overall rate schedule. Furthermore, each insurance contract is different, which means each will reimburse a different percentage of the clinic’s standard rate for any particular service. But, the clinic still bills the same “full amount” for each service (i.e., each individual CPT code), regardless of which insurance company is receiving the bill. This is why the clinic is not always paid the full amount.
2. Know your payer fee schedules—and set your clinic fee schedule accordingly.
So, assuming that (1) each payer has a different rate schedule, and (2) your clinic has—or should have—only one overall fee schedule, it’s important to ensure that your clinic’s fee schedule accounts for the maximum payment from each insurance. For example, if workers’ comp pays $25 per manual therapy code, and BCBS pays $18, then your clinic fee schedule better reflect at least $25; otherwise, you won’t get the maximum payment for your services.
Clinics must also account for out-of-network benefits. Out-of-network insurances usually pay based on either:
- a percentage of what is billed, or
- a different (usually higher) fee schedule.
So, as you create your clinic’s fee schedule, I suggest adding an additional 25-40% to your lowest payment rates to make sure you never leave money on the table.
3. Be mindful of payment reduction rules.
Over the years, payers—Medicare in particular—have introduced a lot of regulations that have ultimately led to reduced reimbursements. Multiple Procedure Payment Reduction (MPPR) was a big one. After that went into effect, CMS stopped paying claims in full when a PT, OT, or SLP performed more than one related procedure on a patient during the same visit. As you evaluate and negotiate your various payer contracts—something you should be doing on a consistent basis—pay attention to these rules. After all, while the fee schedule may look fine and dandy, there’s a chance you may not come out ahead if you’re hit with too many reductions. And if that’s the case, then you should probably think seriously about whether it’s actually in your practice’s best interest to keep your contract with that payer.
4. Don’t underestimate the financial impact of patient payments.
Patient financial responsibility technically doesn’t have any bearing on your fee schedule. However, it’s worth noting that because the patient often is responsible for a percentage of the bill—especially with the proliferation of high-deductible health plans (HDHPs) in recent years—it definitely behooves your practice to collect patient copays, coinsurances, and deductibles upfront. After all, if you fail to collect that amount from the patient directly, then you’re automatically reducing the total amount of payment you receive. If that’s not enough to motivate you to make upfront collection a priority, consider this: only 21% of patient balances that aren’t collected at the point of service are ever collected. I don’t know about you, but I don’t like those odds.
To make things easier on you and your staff, consider using the phrase, “How would you like to pay today? Credit card, cash, or check?,” rather than “Would you like to pay your copay today?” That simple change in phrasing could make a big difference in your practice’s collection rates
While you may not be able to control your payers’ reimbursement rates, you can set your practice up to get the most out of its fee schedule by ensuring it accounts for every patient you serve—whether that patient is in-network, out-of-network, or self-pay. To learn more about the trends impacting rehab therapists most—including frustrations and motivations, financial pressures and strategies, and evolving technology preferences—be sure to download the full State of Rehab Therapy report here.